
Table of Contents
Breastfeeding mums often face headaches, postpartum aches, or muscle pain, but not all painkillers are breastfeeding-friendly. Your baby’s health depends on what passes into your milk, so let’s explore safe pain relievers for breastfeeding moms backed by science and practical tips.
Common concerns include:
- Will the medication harm my baby?
- Are there safer alternatives?
- How do I balance pain relief with my baby’s health?
Why Medication Safety Matters During Breastfeeding
Many pain relievers pass into breast milk, potentially affecting your baby’s health. Understanding how medications transfer into breast milk can help you make an informed choice.
How Medications Transfer Into Breast Milk
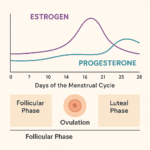
- The extent to which drugs enter breast milk depends on their molecular size, solubility, and half-life.
- Lipid-soluble drugs (fat-loving drugs) tend to transfer more readily.
- The highest drug concentration in milk occurs 1-2 hours after ingestion.
- Premature or newborn babies metabolise drugs slower, making them more sensitive.
Key Factors Affecting Drug Safety in Breastfeeding
- Dosage & Frequency – Higher doses increase the risk of transfer.
- Infant’s Age & Weight – Newborns have an immature liver, making drug metabolism slower.
- Mother’s Metabolism – How quickly your body breaks down the medication affects its presence in milk.
Research published in American Family Physician (2022) states that most common pain relievers, including ibuprofen and acetaminophen, are safe for breastfeeding .
Top Safe Pain Relievers for Breastfeeding Moms
The two safest and most commonly recommended over-the-counter (OTC) pain relievers for breastfeeding moms are:
Acetaminophen (Paracetamol, Tylenol)
Studies have shown that breast-feeding during maternal treatment with paracetamol (acetaminophen) should be regarded as being safe
- Safety: Recognized as the first-line pain reliever for breastfeeding mothers .
- Usage: Used for mild to moderate pain and fever relief.
- Dosage: Up to 1000mg every 6 hours (max 4000mg/day).
- Side Effects: Minimal when used at recommended doses.
- Breast Milk Transfer: Very low, considered safe by the LactMed Database (NIH, 2023).
Ibuprofen (Advil, Motrin)
According to the NHS & Studies in Pediatric Drugs have shown ibuprofen to be not only compatible with breastfeeding, but also extremely safe due to poor transfer into milk and safety in infants and must be preferred for long term treatment.
- Safety: Preferred NSAID for breastfeeding moms due to minimal milk transfer.
- Usage: Effective for inflammation, muscle pain, and fever.
- Dosage: 200-400mg every 4-6 hours (max 1200mg/day).
- Side Effects: Mild stomach irritation in some cases.
- Breast Milk Transfer: Less than 1% of ibuprofen enters breast milk .
Stronger Pain Relief Options
Opioids: For severe pain, the opiates are the preferred method of treatment. Morphine, codeine, hydrocodone, fentanyl, and hydromorphone have been determined, by several studies, to be moderately safe for breastfeeding women.
A study published in American Family Physician (2022) found that If an oral opioid is required for pain control, hydrocodone or morphine is preferred.
- According to the NHS :Morphine does get into breast milk, but usually in pretty small amounts. If you’re taking a low dose for just a short period, it’s unlikely to cause any problems for your little one.”
- According to the study in LactMed® found that Codeine isn’t usually recommended due to concerns about how some people metabolize it, potentially leading to high levels in breast milk and causing drowsiness or breathing problems in the baby.
- Dihydrocodeine: It is a weak opioid. It is the first choice if you need stronger pain relief than paracetamol or ibuprofen whilst breastfeeding, due to your body processes it differently to codeine.
Medications to Avoid While Breastfeeding
Some pain relievers pose risks to infants due to their ability to transfer into breast milk in higher concentrations.
Aspirin (Acetylsalicylic Acid)
- Risk: Increases the risk of Reye’s Syndrome, a rare but serious condition.
- Recommendation: Avoid unless specifically prescribed.
Codeine & Opioids (Hydrocodone, Oxycodone, Tramadol)
According to the U.S. Food and Drug Administration :Codeine & Opioids are restricted in breastfeeding mothers because of patients who are ultra-rapid metabolizers risk exposing infants to excessively high amounts of active metabolites, sedation, and respiratory depression especially in tramadol and codeine.
- Risk: May cause drowsiness, breathing issues, and dependency in infants.
- Recommendation: Only use under strict medical supervision.
Naproxen (Aleve, Naprosyn)
- Risk: Long half-life increases the baby’s exposure.
- Recommendation: Short-term use only if no alternatives exist.
Natural & Non-Medicinal Pain Relief Options
If you prefer to avoid medications, natural alternatives can help:
Heat & Cold Therapy
- Hot compress: according to the study in 2018 in Scientific Reports found that a warm compress eases muscle cramps relieves muscle stiffness, cramps, and joint pain.
- Cold packs: According to the study in Journal of Rehabilitation Medicine found that use of cold packs Reduce swelling and inflammation, ideal for postpartum recovery.
Gentle Exercises & Stretches
- Postpartum yoga and light stretching help reduce muscle tension.
- Pelvic floor exercises aid in postpartum pain recovery.
Safe Herbal Remedies
Magnesium Supplements – Can ease migraines and muscle pain
Turmeric (Curcumin): curcumin extract showed benefits in treating osteoarthritic pain and has anti-inflammatory, but consult a doctor for dosage.
Ginger tea :Ginger is natural pain reliever, helps with bloating and nausea.
Safety Guidelines for Medication Use
To ensure safe pain relief during breastfeeding:
Use Trusted Apps: LactMed (NIH) and BabyTracker offer real-time safety checks.
Time It Right: Take pills right after nursing.
Consult Your GP: Always check with a healthcare provider.
Conclusion: Safe Pain Relievers for Breastfeeding Moms
Finding safe pain relief while breastfeeding involves balancing your well-being with your baby’s health. Options like paracetamol and ibuprofen are generally considered safe, but it’s crucial to use the lowest effective dose and consult your healthcare provider for personalised advice. In situations where stronger pain relief is needed, opioids might be considered, but they should be used with caution and under strict medical supervision. Remember, too, that non-medicinal approaches can be beneficial and may, in some cases, prevent you from the needing more intense prescription drugs. By staying informed and consulting with healthcare professionals, you can manage pain effectively while continuing to provide the best for your baby.
FAQS :Safe Pain Relievers for Breastfeeding Moms
Can I take Tylenol while breastfeeding?
Yes, acetaminophen (Tylenol) is considered safe for nursing moms and is commonly recommended
Is ibuprofen safe for breastfeeding moms?
Yes, ibuprofen (Advil, Motrin) is safe, as it transfers minimally into breast milk and has no reported effects on infants.
Can I use Voltaren gel while breastfeeding?
Yes, topical NSAIDs like diclofenac (Voltaren) have low systemic absorption, making them safer alternatives (LactMed, 2023).
What can I take for migraines while breastfeeding?
First-line: Acetaminophen or ibuprofen.
Alternative: Magnesium supplements and cold compresses.
Avoid: Triptans without consulting a doctor.









Hello. splendid job. I did not imagine this. This is a great story. Thanks!