Table of Contents
Introduction: You Can Stop Taking Antibiotics as Soon as You Feel Better
What are Antibiotics?
Antibiotics are medications used to treat bacterial infections by either killing the bacteria or slowing their growth. They are a critical tool in modern medicine, allowing healthcare providers to effectively manage a wide range of infectious diseases. Antibiotics work by targeting specific processes or structures within bacterial cells, disrupting their ability to function and reproduce.
The Importance of Completing the Full Antibiotic Course
One of the most important principles of proper antibiotic use is completing the full course of treatment as prescribed by a healthcare provider. This means taking all of the doses of the antibiotic, even if you start feeling better before the course is finished. Failing to complete the full course can allow some bacteria to survive, leading to the potential development of antibiotic-resistant infections.
Myth: You Can Stop Taking Antibiotics as Soon as You Feel Better
A common myth is that you can stop taking antibiotics as soon as you start feeling better. This is incorrect and can be dangerous. Antibiotics need to be taken for the full prescribed duration in order to eliminate the infection completely. Stopping too soon can allow the remaining bacteria to multiply and the infection to return, potentially in a more resistant form.
The Dangers of Antibiotic Resistance
Antibiotic resistance is a growing global health concern. When bacteria are exposed to antibiotics but not completely eliminated, they can develop defenses against those antibiotics. This makes future infections caused by those bacteria much more difficult to treat, as the standard antibiotic therapies will no longer be effective. Improper antibiotic use, such as not completing the full course, is a major contributor to the rise of antibiotic-resistant bacteria.
Antibiotic Use and Infections
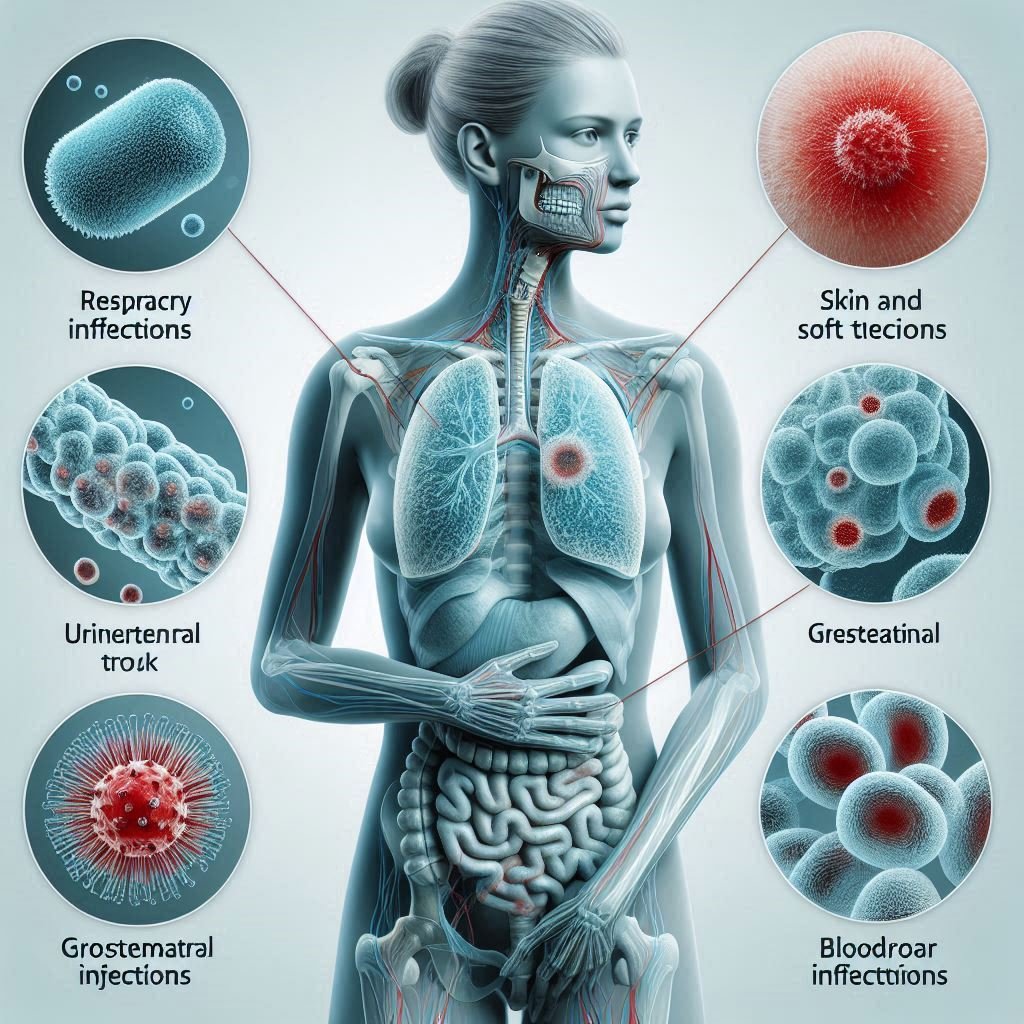
Antibiotics are used to treat a variety of bacterial infections, including:
- Respiratory infections (e.g., pneumonia, bronchitis)
- Skin and soft tissue infections (e.g., cellulitis, impetigo)
- Urinary tract infections
- Gastrointestinal infections (e.g., traveler’s diarrhea)
- Bloodstream infections (e.g., sepsis)
It’s important to note that antibiotics are only effective against bacterial infections and have no impact on viral infections, such as the common cold or the flu. Using antibiotics for viral infections is not only ineffective, but can also contribute to the development of antibiotic resistance.
Proper Antibiotic Dosage and Administration
Following the dosage instructions provided by healthcare providers is crucial for the effective treatment of bacterial infections. Taking the correct amount of the antibiotic at the right intervals helps ensure that sufficient levels of the medication are maintained in the body to eliminate the infection. Failing to adhere to the prescribed dosage can lead to suboptimal treatment and the potential for antibiotic resistance to develop.
Antibiotic Side Effects and Risks
While antibiotics are generally safe and well-tolerated, they can sometimes cause side effects. Common side effects of antibiotic use include:
- Gastrointestinal issues (e.g., nausea, diarrhea, abdominal pain)
- Allergic reactions (e.g., rash, hives, difficulty breathing)
- Disruption of the gut microbiome, leading to infections like Clostridioides difficile (C. diff)
It’s important for patients to monitor for any adverse effects and report them to their healthcare provider. In some cases, the antibiotic may need to be changed or the dosage adjusted to better manage the side effects.
Monitoring for Side Effects and Seeking Medical Attention
Patients should be vigilant for any side effects that may occur during antibiotic treatment and report them to their healthcare provider. Prompt medical attention is especially important for severe or concerning side effects, such as severe diarrhea, difficulty breathing, or signs of an allergic reaction. Early intervention can help mitigate the risks and ensure appropriate management of any adverse effects.
FAQS: You Can Stop Taking Antibiotics as Soon as You Feel Better
Why is it important to finish the entire course of antibiotics?
Antibiotic Resistance: Antibiotic resistance is a growing problem, and finishing your entire course of antibiotics helps to prevent it. When bacteria are exposed to antibiotics, they can develop resistance, making them harder to treat.
What are the risks of stopping antibiotics early?
Antibiotic Resistance: Stopping antibiotics early can contribute to the development of antibiotic-resistant bacteria, making future infections more difficult to treat.
What if I experience side effects from antibiotics?
Do Not Stop Taking Antibiotics Without Medical Advice: Stopping antibiotics early can lead to the risks mentioned above.









Valuable info. Lucky me I discovered your site unintentionally, and I’m stunned why this accident did not happened in advance! I bookmarked it.