
Table of Contents
What is a Migraine?
According to the National Institute of Neurological Disorders and Stroke :
- Migraine is more than a severe headache; it is a recurring neurological condition with a range of symptoms.
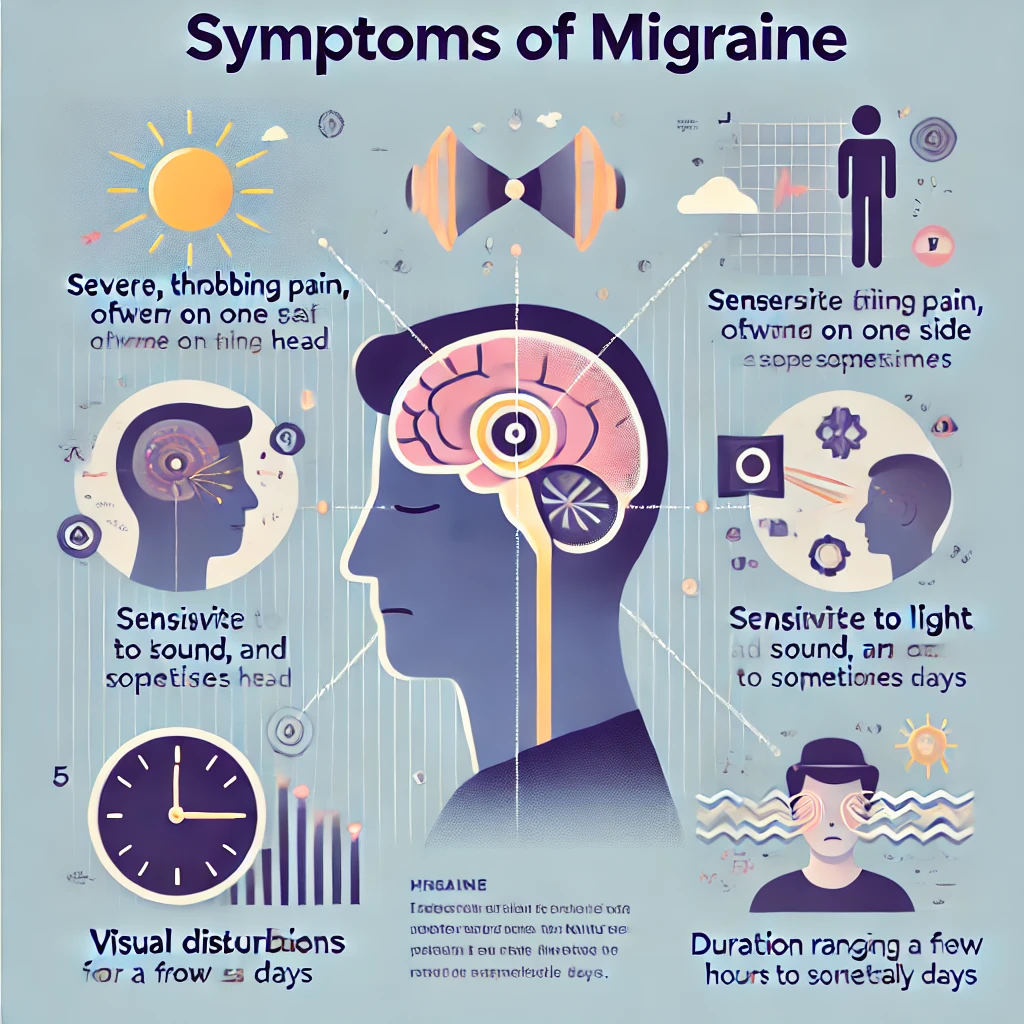
- Symptoms vary from person to person and can include:
- Throbbing, one-sided head pain
- Nausea and vomiting
- Sensitivity to light, sound, and smells
- Mood changes
- Extreme fatigue
- Migraine attacks can last from hours to days and often interfere with daily life.
- The pain is linked to abnormal brain activity involving nerves, chemicals, and blood vessels.
- Some people experience attacks at predictable times, such as before menstruation or after a stressful week.
- Between attacks, individuals may still have symptoms like trouble focusing, anxiety, depression, sleep issues, or chills.
Migraines affect millions of people worldwide, with varying frequency and severity. Some individuals experience migraines occasionally, while others suffer from chronic migraines, defined as 15 or more headache days per month.
According to the American Academy of Family Physicians
- Over 28 million Americans suffer from migraines
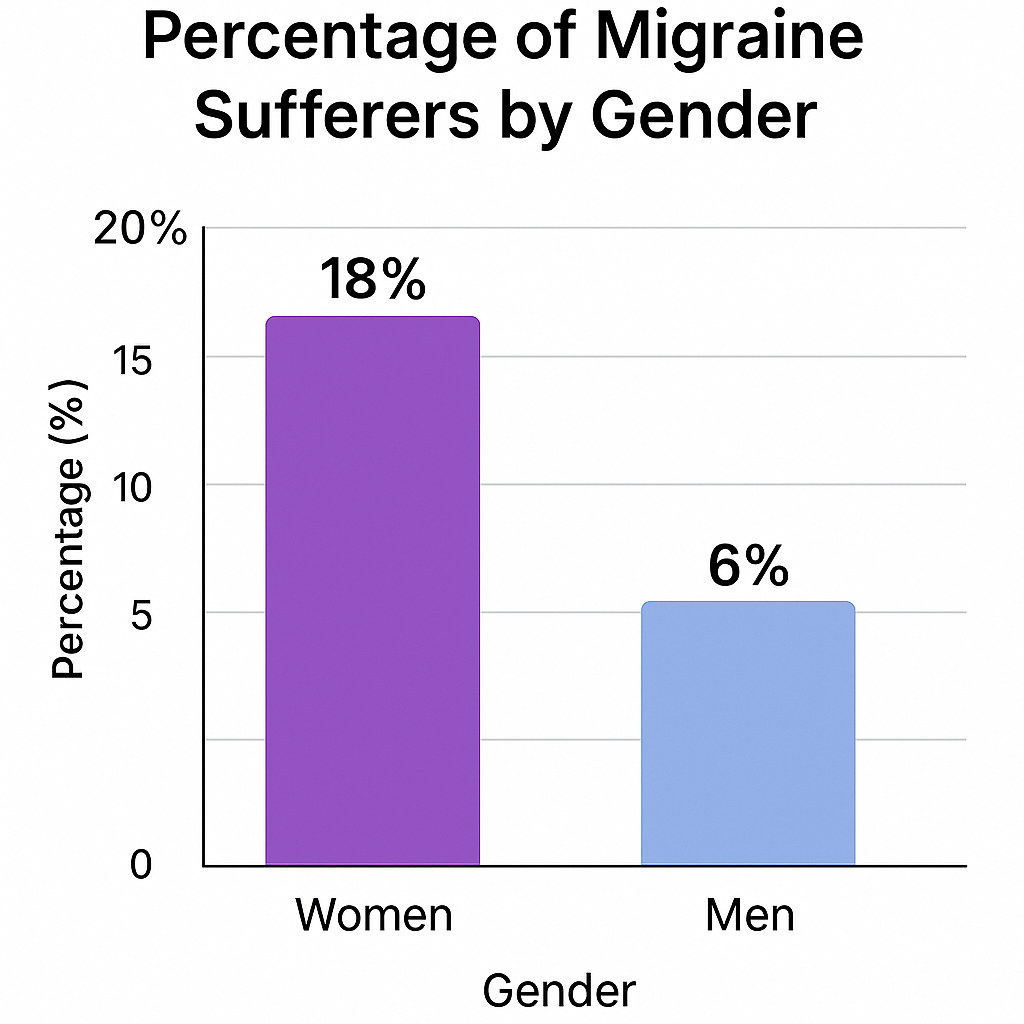
- 18% of women vs 6% of men have migraines
- 38% of migraine sufferers need preventive therapy
- Only 3–13% actually use preventive treatment
The Migraine Spectrum
It’s important to understand that migraines exist on a spectrum. At one end, there are mild migraines that cause discomfort but don’t significantly disrupt daily activities. At the other end, there are severe migraines that can be completely debilitating, forcing individuals to retreat to dark, quiet rooms for extended periods.
Symptoms of the migraine
The Phases of a Migraine
According to the Neurology Clinical Practice (2025) ,a migraine attack typically progresses through four phases, although not everyone experiences all phases:
- Prodrome (Pre-headache) Symptoms:
- Mood changes (depression, irritability, or euphoria)
- Food cravings
- Increased thirst and urination
- Neck stiffness
- Yawning
- Fatigue or low energy
2. Aura Symptoms (experienced by about 25% of migraine sufferers):
- Visual disturbances (seeing flashing lights, zigzag lines, or blind spots)
- Sensory changes (tingling or numbness in face or extremities)
- Speech difficulties
- Motor weakness (in hemiplegic migraine)
- Vertigo or dizziness
3.Headache Phase Symptoms:
- Intense, throbbing pain, often on one side of the head
- Increased pain with physical activity or movement
- Nausea and vomiting
- Sensitivity to light (photophobia)
- Sensitivity to sound (phonophobia)
- Sensitivity to smells (osmophobia)
- Blurred vision
- Lightheadedness or fainting
- Neck pain
4.Postdrome (Post-headache) Symptoms:
- Fatigue
- Difficulty concentrating
- Mild confusion
- Weakness
- Dizziness
- Mood changes (depression or euphoria)
Causes and Triggers of migraines
What are the common causes of migraines?
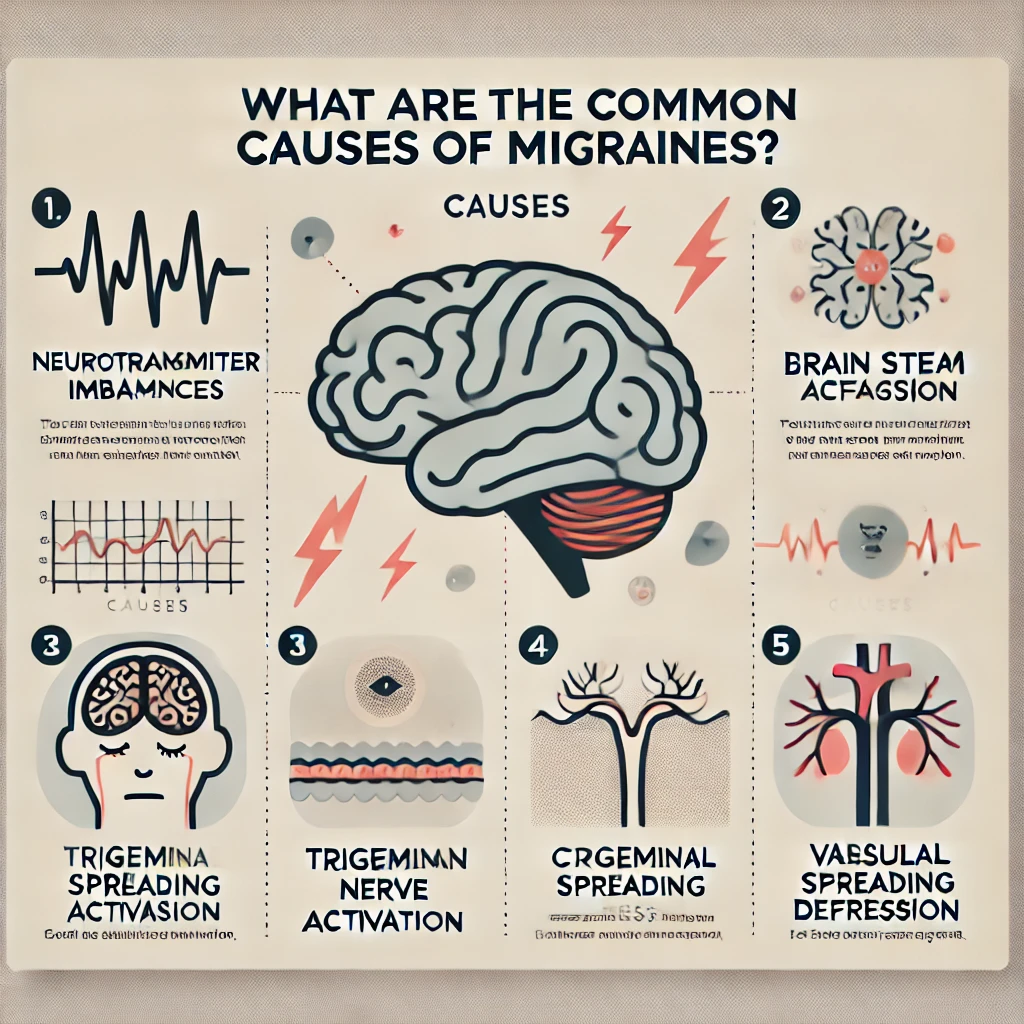
Migraines are believed to result from a complex interplay of genetic, environmental, and neurological factors. Some of the primary causes include:
- Neurotransmitter Serotonin (5-HT) Imbalance: According to the study in Frontiers in Molecular Neuroscience (2025) published that Changes in brain chemicals, particularly serotonin levels, are thought to play a significant role in migraine development. Serotonin helps regulate pain in the nervous system, and fluctuations in its levels can trigger migraines.
- Brain Stem Changes: According to the study in The Journal of Headache and Pain (2019) reported that the brain stem, which connects the brain to the spinal cord, plays a crucial role in processing pain signals. Alterations in brain stem function may contribute to migraine onset.
- Trigeminal Nerve Activation: According to the study in The Journal of Headache and Pain stated that the trigeminal nerve, which is responsible for sensation in the face and head, may become overstimulated, leading to the release of pain-causing substances.
- Cortical Spreading Depression: According to the study in Cephalalgia published that Cortical spreading depression involves a wave of brain signaling that spreads across the cerebral cortex, potentially triggering the pain and other symptoms associated with migraines.
- Vascular Changes: According to the study in Journal of Cerebral Blood Flow & Metabolism published that Vascular Changes no longer considered the primary cause, changes in blood flow in the brain may contribute to migraine symptoms.
How do environmental factors contribute to migraines?
Environmental factors play a significant role in triggering migraines for many sufferers. Some key environmental factors include:
- Weather Changes: According to the study in Environment International reported that Many migraine sufferers report sensitivity to changes in barometric pressure, temperature, or humidity. Storms, high winds, and extreme temperatures can all potentially trigger migraines.
- Light Exposure: A study in a review published in Headache (2022) stated that bright or flickering lights, including fluorescent lights and sunlight glare, can trigger migraines in sensitive individuals. This sensitivity to light is known as photophobia.
- Noise Pollution(Phonophobia): A study in European Journal of Neurology discusses noise as a common migraine trigger and highlights behavioral strategies for managing trigger exposure, emphasizing the role of central sensitization and limbic system involvement in noise sensitivity during migraine.
- Strong Odors: A study in Cephalalgia 2017 reported that Certain smells, such as perfumes, cleaning products, or cigarette smoke, can trigger migraines in sensitive individuals. This is known as osmophobia.
- Altitude Changes: According to the study published in Current pain & head reports reported that rapid changes in altitude, such as during air travel or mountain climbing, can trigger migraines in some people.
- Air Quality: According to the study in Annals of Indian Academy of Neurology reported that Poor air quality, including high levels of pollutants or allergens, may contribute to migraine occurrence in sensitive individuals.
The role of genetics in migraine development
Genetics plays a significant role in an individual’s susceptibility to migraines. Research has shown that migraines tend to run in families, suggesting a strong genetic component. Some key points about the genetic aspects of migraines include:
- Family History: According to the study by Nature genetics reported that If one or both parents suffer from migraines, their children have a higher likelihood of developing the condition. The risk increases if both parents are affected.
- Genetic Variants: According to the study in Nature genetics reported that Several genes have been identified that may increase susceptibility to migraines. These genes are often related to brain function, blood vessel regulation, or pain processing.
- Rare Genetic Disorders: According to the study in Journal of Neurology, Neurosurgery, and Psychiatry reported that Some rare genetic disorders, such as familial hemiplegic migraine, are directly linked to specific genetic mutations and cause severe forms of migraine.
- Epigenetics: According to the study in BMC Genomics reported that Environmental factors can influence how genes are expressed, potentially affecting migraine susceptibility and frequency.
- Gene-Environment Interactions: According to the study in International Journal of Molecular Sciences reported that An individual’s genetic makeup may influence how they respond to environmental triggers, explaining why some people are more sensitive to certain migraine triggers than others.
Common triggers for migraine: food, stress, hormones, etc.
Some common migraine triggers include:
- Food and Drink:
- According to the Nutrients ,Caffeine (both excessive consumption and withdrawal) is related to chronic migraine progression.
- According to the study in Alcohol and Alcoholism, Tyramine, phenols, and sulfites in red wine provoke migraine via vasodilation and trigeminal activation.
- According to the study in Nutrients ,Aged cheeses and processed meats containing nitrates .Nitrates → nitric oxide → cerebral vasodilation and neuronal sensitization in susceptible individuals.
- According to the study in Dermatitis Artificial sweeteners like aspartame has been linked to the migraines.
- According to the study in Nutrients reported that Monosodium glutamate (MSG) may trigger migraines because it affects the brain’s glutamate system, activating pain receptors and making nerve cells more sensitive to pain.
- According to the study in Nutrients Chocolate (for some individuals) has been linked to migraines.
- Skipping meals or fasting is also associated with migraine according to the Current Pain Headache Reports .But this study also shows benefits of fasting for migraine patients.
- Stress: According to the study published in BMC Neurology reported that Stress is the most frequently self-reported trigger for migraine attacks, with evidence suggesting that both acute and chronic stress can precipitate migraine onset.
- Emotional stress
- Physical stress
- Work-related stress
- Major life changes
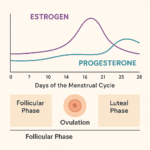
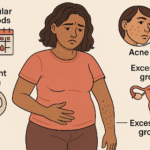
- Hormonal Changes: According to the study published in Lancet Neurology has been showed Estrogen withdrawal premenstrually sensitizes trigeminal pathways.
- Menstrual cycle fluctuations
- Pregnancy
- Menopause
- Hormonal contraceptives
- Sleep Disturbances:
- Lack of sleep
- Too much sleep
- Changes in sleep patterns
- Jet lag
- Physical Factors:
- Intense physical exertion
- Sexual activity
- Head trauma
- Medications:
- Certain blood pressure medications
- Oral contraceptives
- Overuse of pain relievers (rebound headaches)
- Sensory Stimuli:
- Bright or flickering lights
- Loud noises
- Strong smells
- Weather Changes:
- Barometric pressure fluctuations
- Temperature changes
- Storms
- Dehydration:
- Not drinking enough water
- Excessive sweating without proper hydration
Diagnosis of the Migraine
How are migraines diagnosed?
Diagnosing migraines can be challenging as there is no specific test that can definitively identify them. Instead, healthcare providers rely on a combination of methods:
- Medical History:
- Detailed description of symptoms
- Family history of migraines
- Triggers and patterns of attacks
- Physical and Neurological Examination:
- Checking vital signs
- Testing reflexes, coordination, and sensation
- Examining the head, neck, and eyes
- Headache Diary Review:
- Frequency and duration of headaches
- Associated symptoms
- Potential triggers
- Diagnostic Criteria:
- The International Headache Society’s International Classification of Headache Disorders (ICHD) provides specific criteria for diagnosing various types of migraines.
- Imaging Studies (to rule out other conditions):
- MRI (Magnetic Resonance Imaging)
- CT (Computed Tomography) scan
- Blood Tests:
- To rule out other conditions that might cause headaches
- Specialized Tests (in some cases):
- Lumbar puncture (spinal tap)
- EEG (Electroencephalogram)
The diagnosis of migraines is primarily clinical, based on the patient’s reported symptoms and the exclusion of other potential causes. This is why accurate symptom reporting and maintaining a migraine journal are crucial for diagnosis.
The importance of keeping a migraine journal
A migraine journal is an invaluable tool for both patients and healthcare providers in the diagnosis and management of migraines. Here’s why it’s so important:
- Identifying Patterns:
- Frequency and duration of migraines
- Time of day or month when migraines occur
- Recognizing Triggers:
- Foods, activities, or environmental factors that precede migraines
- Tracking Symptoms:
- Progression of symptoms through different migraine phases
- Intensity and location of pain
- Monitoring Treatment Efficacy:
- Response to different medications or treatments
- Side effects of medications
- Providing Accurate Information to Healthcare Providers:
- Detailed history for more accurate diagnosis
- Data for adjusting treatment plans
- Empowering Patients:
- Increases understanding of one’s condition
- Aids in predicting and preparing for migraine attacks
A comprehensive migraine journal should include:
- Date and time of migraine onset and end
- Intensity of pain (often on a scale of 1-10)
- Location of pain
- Associated symptoms
- Potential triggers (food, stress, weather, etc.)
- Medications taken and their effectiveness
- Impact on daily activities
Many digital apps are now available to help patients keep detailed migraine journals, making it easier to track and analyze migraine patterns over time.
Types of migraines (e.g., aura, without aura, etc.)
The main types of migraines include:
- Migraine without Aura (Common Migraine):
- Most frequent type of migraine
- Characterized by the typical headache symptoms without the preceding aura
- May still have prodrome and postdrome symptoms
- Migraine with Aura (Classic Migraine):
- About 25% of migraine sufferers experience aura
- Visual, sensory, or speech disturbances precede or accompany the headache
- Aura typically lasts 20-60 minutes
- Chronic Migraine:
- Headaches occur on 15 or more days per month for more than three months
- At least eight of these headache days meet criteria for migraine
- Hemiplegic Migraine:
- Rare and severe form of migraine with aura
- Includes temporary motor weakness on one side of the body
- Can be familial (genetic) or sporadic
- Retinal Migraine:
- Characterized by temporary vision loss or disturbances in one eye
- Usually accompanied by a headache
- Vestibular Migraine:
- Prominent vestibular symptoms (vertigo, dizziness, balance problems)
- May or may not be accompanied by headache
- Basilar-type Migraine:
- Aura symptoms originating from the brainstem
- May include double vision, vertigo, and difficulty speaking
- Abdominal Migraine:
- More common in children
- Characterized by abdominal pain, nausea, and vomiting
- May or may not be accompanied by head pain
- Menstrual Migraine:
- Occurs in relation to the menstrual cycle
- Can be pure menstrual migraine (exclusively around menstruation) or menstrually-related migraine (also occurs at other times)
- Status Migrainosus:
- A severe, long-lasting migraine attack
- Symptoms persist for more than 72 hours
Healthcare providers use the International Classification of Headache Disorders (ICHD) to diagnose specific types of migraines based on detailed criteria for each type. This classification system is regularly updated as new research provides more insights into migraine disorders.
Migraine Management: Treatment Options, Prevention, and Lifestyle Changes
Effective migraine management involves a multi-faceted approach that includes acute treatment, preventive strategies, and lifestyle modifications. This comprehensive guide will explore various aspects of migraine management to help sufferers gain better control over their condition and improve their quality of life.
Medications for migraine relief: over-the-counter, prescription, and natural remedies
Migraine medication can be broadly categorized into two types: acute treatments (taken during a migraine attack) and preventive treatments (taken regularly to reduce the frequency and severity of migraines).
- Acute Treatments:
a) Over-the-counter (OTC) medications:- Nonsteroidal anti-inflammatory drugs (NSAIDs): Ibuprofen, Aspirin, Naproxen Acetaminophen (Paracetamol)Combination drugs: Aspirin + Acetaminophen + Caffeine
- Triptans (e.g., Sumatriptan, Rizatriptan)
- Ergotamines
- Anti-nausea medications (e.g., Metoclopramide)
- Gepants (e.g., Ubrogepant, Rimegepant)
- Ditans (e.g., Lasmiditan)
- Preventive Treatments:
a) Prescription medications:- Beta-blockers (e.g., Propranolol, Metoprolol)Antidepressants (e.g., Amitriptyline, Venlafaxine)Anticonvulsants (e.g., Topiramate, Valproic acid)Calcitonin gene-related peptide (CGRP) monoclonal antibodies (e.g., Erenumab, Fremanezumab)Botulinum toxin A (Botox) injections
- Magnesium
- Riboflavin (Vitamin B2)
- Coenzyme Q10
- Feverfew
- Butterbur
Lifestyle changes for managing migraines: diet, exercise, sleep, etc.
These changes can help reduce the frequency and severity of migraines:
- Diet:
- Identify and avoid personal food triggers
- Maintain regular meal times to prevent hypoglycemia
- Stay hydrated
- Limit caffeine and alcohol intake
- Consider following a migraine-specific diet (e.g., low tyramine diet)
- Exercise:
- Engage in regular, moderate exercise (e.g., walking, swimming, cycling)
- Practice relaxation techniques like yoga or tai chi
- Be cautious with high-intensity workouts, which can trigger migraines in some people
- Sleep:
- Maintain a consistent sleep schedule
- Create a relaxing bedtime routine
- Ensure a comfortable sleep environment (dark, quiet, cool)
- Address sleep disorders like sleep apnea
- Stress Management:
- Practice stress-reduction techniques (e.g., meditation, deep breathing exercises)
- Consider cognitive-behavioral therapy (CBT)
- Time management and prioritization of tasks
- Environmental Adjustments:
- Use anti-glare screens and proper lighting to reduce eye strain
- Wear sunglasses outdoors to protect from bright light
- Use earplugs or noise-cancelling headphones in loud environments
- Hormonal Management:
- For menstrual-related migraines, consider hormonal birth control or hormone therapy under medical supervision
- Posture and Ergonomics:
- Maintain good posture to reduce neck and shoulder tension
- Ensure ergonomic work setups to prevent strain
Alternative therapies for migraine relief: acupuncture, massage, etc.
Many migraine sufferers find relief through alternative and complementary therapies. While scientific evidence varies for these treatments, many report significant benefits:
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. Some studies suggest it may help reduce migraine frequency and intensity.
- Massage Therapy: Regular massages, especially focusing on the neck, shoulders, and head, can help reduce tension and may decrease migraine frequency.
- Biofeedback: This technique helps individuals learn to control certain bodily processes, such as muscle tension and heart rate, which may help manage migraines.
- Chiropractic Care: Spinal manipulation may help some people with migraines, particularly those with neck tension or misalignment.
- Herbal Remedies: Besides feverfew and butterbur, other herbs like ginger and peppermint have been used traditionally for headache relief.
- Essential Oils: Some people find relief using essential oils like peppermint, lavender, or eucalyptus for aromatherapy or topical application.
- Transcutaneous Electrical Nerve Stimulation (TENS): This therapy uses mild electrical currents to stimulate nerves and may help reduce pain.
- Cognitive Behavioral Therapy (CBT): While primarily used for stress management, CBT can also help individuals cope with pain and develop strategies for managing migraines.
It’s important to consult with a healthcare provider before starting any alternative therapies, especially to ensure they don’t interact with other treatments or underlying health conditions.
The role of mindfulness and relaxation techniques in migraine management
These practices can help reduce stress, a common migraine trigger, and may even help in pain management during an attack:
- Mindfulness Meditation: This practice involves focusing on the present moment without judgment. Regular mindfulness practice may help reduce the frequency and severity of migraines.
- Progressive Muscle Relaxation: This technique involves systematically tensing and relaxing different muscle groups, helping to reduce overall body tension.
- Deep Breathing Exercises: Techniques like diaphragmatic breathing can help activate the body’s relaxation response, potentially reducing migraine intensity.
- Guided Imagery: This practice involves using mental images to promote relaxation and may help manage pain during a migraine attack.
- Body Scan Meditation: This mindfulness technique involves systematically focusing attention on different parts of the body, promoting relaxation and body awareness.
- Mindful Movement: Practices like yoga or tai chi combine physical movement with mindfulness, potentially helping with both stress reduction and physical tension.
- Biofeedback: While also considered an alternative therapy, biofeedback incorporates mindfulness and relaxation principles to help individuals control physiological processes.
Incorporating these techniques into daily life can help manage stress levels and potentially reduce migraine frequency. During a migraine attack, these practices may also help in coping with pain and associated symptoms.
Strategies for preventing migraines: stress reduction, relaxation techniques, etc.
Preventing migraines is a crucial aspect of management. While some strategies overlap with lifestyle changes and relaxation techniques, here are some specific prevention strategies:
- Trigger Avoidance: Identify and avoid personal migraine triggers through careful tracking and gradual elimination.
- Stress Management:
- Regular practice of relaxation techniques
- Time management and prioritization
- Setting realistic goals and expectations
- Preventive Medications: Consistent use of prescribed preventive medications as directed by a healthcare provider.
- Regular Exercise: Engaging in moderate, regular exercise can help reduce migraine frequency.
- Consistent Sleep Schedule: Maintaining regular sleep and wake times, even on weekends.
- Dietary Considerations:
- Regular, balanced meals
- Staying hydrated
- Limiting known dietary triggers (e.g., caffeine, alcohol, certain additives)
- Hormone Management: For those with menstrual-related migraines, strategies may include hormonal birth control or perimenstrual preventive medication.
- Complementary Therapies: Regular use of beneficial alternative therapies like acupuncture or massage.
- Environmental Management:
- Using blue light filters on digital devices
- Ensuring proper lighting and ergonomics in work and home environments
- Using air purifiers if sensitive to environmental pollutants
- Stress-Reduction Techniques:
- Mindfulness practices
- Cognitive-behavioral therapy
- Regular relaxation exercises
- Weather Preparation: For those sensitive to weather changes, monitoring forecasts and preparing accordingly (e.g., staying indoors during high-pressure days).
- Supplementation: Under medical supervision, using supplements that may help prevent migraines (e.g., magnesium, riboflavin, CoQ10).
How to manage migraines during different life stages (e.g. pregnancy, menopause, etc.)
Migraine management often needs to be adjusted during different life stages, particularly for women due to hormonal influences:
- Pregnancy:
- Many women experience improvement in migraines during pregnancy, especially after the first trimester
- Focus on non-pharmacological treatments when possible
- Consult with healthcare providers about safe medication options if needed
- Pay extra attention to sleep, hydration, and stress management
- Menopause:
- Migraines often change during perimenopause and menopause
- Hormone replacement therapy may help some women but exacerbate migraines in others
- Focus on lifestyle management and non-hormonal preventive treatments
- Consider working with a headache specialist familiar with menopause-related changes
- Adolescence:
- Migraines often begin or worsen during puberty
- Education about triggers and lifestyle management is crucial
- Work with pediatric headache specialists for appropriate treatment plans
- Older Adults:
- Be aware of potential medication interactions and side effects
- Consider comorbid conditions when devising treatment plans
- Focus on lifestyle management and non-pharmacological approaches when possible
- During Menstruation:
- Short-term preventive treatment around menstruation may be helpful
- Hormonal birth control may be considered to regulate hormones
- Pay extra attention to sleep, diet, and stress management during this time
In all life stages, it’s crucial to work closely with healthcare providers to ensure safe and effective migraine management strategies.
How to create a migraine-friendly environment at home and in the workplace
Creating environments that minimize potential migraine triggers can significantly aid in management:
- Lighting:
- Use warm, non-flickering lights
- Install dimmer switches
- Use anti-glare filters on computer screens
- Provide access to natural light when possible
- Noise Control:
- Use noise-cancelling headphones or earplugs when needed
- Create quiet zones in the home or workplace
- Air Quality:
- Use air purifiers to reduce allergens and odors
- Avoid strong-smelling cleaning products or air fresheners
- Ergonomics:
- Ensure proper posture with ergonomic chairs and desks
- Position computer screens at eye level to reduce neck strain
- Hydration Stations:
- Keep water easily accessible to promote hydration
- Relaxation Spaces:
- Create areas for short breaks or relaxation exercises
- Temperature Control:
- Maintain a comfortable, consistent temperature
- Provide personal fans or heaters for individual comfort
- Flexible Scheduling:
- When possible, allow for flexible work hours to accommodate migraine management
- Scent-Free Policies:
- Implement and enforce scent-free policies in the workplace
- Emergency Kits:
- Keep migraine medications and comfort items (e.g., eye masks, cold packs) readily available.
Living with Migraines
Migraines are more than just headaches; they can significantly impact every aspect of a person’s life. Understanding how to navigate life with migraines is crucial for maintaining quality of life and overall well-being.
The emotional impact of living with migraines
Living with migraines can take a substantial emotional toll on individuals. The unpredictable nature of migraines can lead to various emotional challenges:
- Anxiety and Depression:
- Fear of the next attack can cause persistent anxiety
- Frequent pain and disability can contribute to depression
- The isolation often accompanying migraines can exacerbate mood disorders
- Frustration and Anger:
- Feeling powerless against the pain
- Frustration with treatment failures or side effects
- Anger at the limitations imposed by migraines
- Guilt:
- Feeling like a burden to family and friends
- Guilt over missed work or social obligations
- Self-blame for perceived inability to control migraines
- Loss of Identity:
- Difficulty maintaining roles (parent, spouse, employee) during attacks
- Feeling defined by the condition rather than personal attributes
- Stress:
- Constant worry about triggering an attack
- Financial stress from medical expenses or lost work
- Relationship stress due to the impact of migraines on daily life
- Grief:
- Mourning the loss of a “normal” life
- Sadness over missed opportunities or experiences
- Low Self-Esteem:
- Feeling inadequate due to limitations imposed by migraines
- Negative self-image related to the inability to control the condition
Addressing these emotional impacts is crucial for overall migraine management. Strategies may include:
- Seeking professional mental health support
- Joining support groups to connect with others who understand
- Practicing self-compassion and mindfulness
- Engaging in activities that boost self-esteem when feeling well
- Educating loved ones about the emotional toll of migraines
Research and Breakthroughs
The field of migraine research is dynamic and rapidly evolving, with new discoveries and treatment options emerging regularly.
The latest research on migraine causes, diagnosis, and treatment
- Migraine Causes:
a) Genetic Research:- Genome-wide association studies (GWAS) have identified over 40 genetic variants associated with migraine risk.Research into familial hemiplegic migraine has uncovered specific gene mutations affecting ion channels and neurotransmitter release.
- Advanced MRI techniques have revealed structural and functional brain differences in migraine patients.Studies have shown altered brain connectivity and activity patterns during different migraine phases.
- The role of calcitonin gene-related peptide (CGRP) in migraine pathophysiology has been a major focus.Research into the interplay between serotonin, dopamine, and other neurotransmitters in migraine is ongoing.
- Migraine Diagnosis:
a) Biomarker Research:- Scientists are searching for reliable blood or cerebrospinal fluid biomarkers for migraine diagnosis and prediction.Potential biomarkers include specific proteins, metabolites, and microRNAs.
- Functional MRI and PET scans are being explored as tools for objective migraine diagnosis.Research into imaging biomarkers that can predict treatment response is ongoing.
- Machine learning algorithms are being developed to analyze patient data and improve diagnostic accuracy.
- AI-powered analysis of brain scans shows promise in differentiating migraine from other headache disorders.
- Migraine Treatment:
a) Targeted Therapies:- CGRP antagonists and monoclonal antibodies have emerged as a major breakthrough in migraine prevention and treatment.Research into other molecular targets, such as pituitary adenylate cyclase-activating polypeptide (PACAP), is ongoing.Non-invasive neuromodulation devices, such as transcranial magnetic stimulation (TMS) and vagus nerve stimulation, are being studied for both acute and preventive treatment.Research is focusing on identifying genetic and clinical factors that can predict treatment response, allowing for more personalized treatment approaches.Studies are exploring the efficacy of combining different treatment modalities, such as medications and neuromodulation.Research into alternative drug delivery methods, such as intranasal sprays and transdermal patches, aims to improve the efficacy and tolerability of migraine medications.
c) Precision Medicine:
d) Combination Therapies:
e) Novel Drug Delivery Methods:
Breakthroughs in migraine treatment: new medications, therapies, and technologies
- CGRP-Targeted Therapies:
- Monoclonal antibodies targeting CGRP or its receptor (e.g., erenumab, fremanezumab, galcanezumab, eptinezumab) have shown significant efficacy in migraine prevention.
- Small molecule CGRP receptor antagonists (gepants) like ubrogepant and rimegepant have been approved for acute migraine treatment.
- Ditans:
- Lasmiditan, a selective 5-HT1F receptor agonist, represents a new class of acute migraine treatments for patients who can’t take triptans.
- Advanced Neuromodulation Devices:
- FDA-approved devices like the Cefaly (external trigeminal nerve stimulation) and gammaCore (non-invasive vagus nerve stimulation) offer non-pharmacological options for migraine treatment.
- Botulinum Toxin:
- While not new, the use of botulinum toxin injections for chronic migraine prevention has been refined and is now widely accepted as an effective treatment option.
- Telemedicine and Digital Health:
- The integration of telemedicine in migraine care has improved access to specialists and allowed for more frequent follow-ups.
- Digital health platforms and apps for migraine tracking and management have become more sophisticated, often incorporating AI for personalized insights.
- Advanced Wearables:
- Wearable devices that can predict or abort migraine attacks are in development, with some already available on the market.
- Precision Medicine Approaches:
- Genetic testing to guide treatment choices is becoming more common, allowing for more personalized treatment plans.
FAQs: Migraine diagnosis and treatment
What is causing migraines?
Migraines can be triggered by a combination of genetic and environmental factors, such as stress, hormonal changes, certain foods, lack of sleep, and sensory stimuli like bright lights or strong smells.
Can you stop a migraine?
While migraines can’t always be stopped, early intervention with medication, resting in a dark and quiet room, and using cold compresses may help alleviate the symptoms.
How to solve migraine?
Managing migraines often involves a combination of medications, lifestyle changes (such as maintaining a regular sleep schedule and staying hydrated), and avoiding known triggers.
What are the 5 C’s of migraines?
The 5 C’s of migraines refer to: Causes, Characteristics, Complications, Control (management strategies), and Care (supportive measures and self-care).









As I web-site possessor I believe the content material here is rattling great , appreciate it for your hard work. You should keep it up forever! Good Luck.