Table of Contents
1. Understanding Conjunctivitis (Pink Eye)
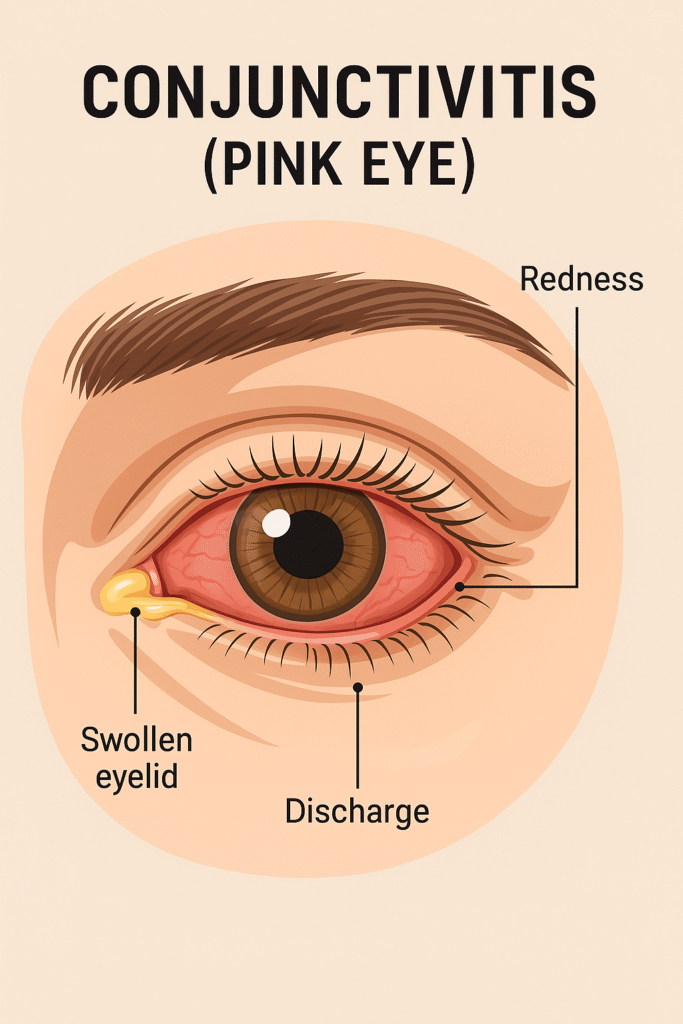
Conjunctivitis, commonly called pink eye, is an inflammation of the conjunctiva—the thin, clear tissue covering the white part of your eye. It can be caused by bacteria, viruses, allergies, or even sexually transmitted infections (STIs) like chlamydial conjunctivitis.
Types of Conjunctivitis (Pink Eye)
- Bacterial Conjunctivitis – Caused by bacteria like Staphylococcus or Streptococcus, leading to thick yellow/green discharge.
- Viral Conjunctivitis – Often linked to colds, with watery discharge and extreme redness.
- Allergic Conjunctivitis – Triggered by pollen, dust, or pet dander, causing itching and swelling.
- Chlamydial Conjunctivitis – An STI-related form, requiring antibiotics like azithromycin (CDC, 2023).

Can Sinus Infections Cause Pink Eye?
Yes! An eye infection from sinus issues (like bacterial sinusitis) can spread bacteria to the eyes, worsening conjunctivitis (American Academy of Ophthalmology ,2024).
2. Symptoms & Diagnosis: When to Worry
Key Symptoms
- Red, itchy, or burning eyes
- Thick discharge (bacterial) vs. watery eyes (viral)
- Crusty eyelids (especially after sleep)
When to See a Doctor
- Severe pain or vision changes
- Symptoms lasting over a week
- High fever (possible systemic infection)
3. Prevalence of Conjunctivitis (Pink Eye) by Age and Gender
Conjunctivitis affects people of all ages, but certain groups are more susceptible. Recent studies highlight key trends in its distribution across different demographics.
Age-Specific Prevalence
Children (0–7 years): The highest incidence occurs in children under seven, particularly between birth and four years.(Azari & Barney, 2013).
Factors like poor hand hygiene, school exposure, and viral infections contribute to this trend.
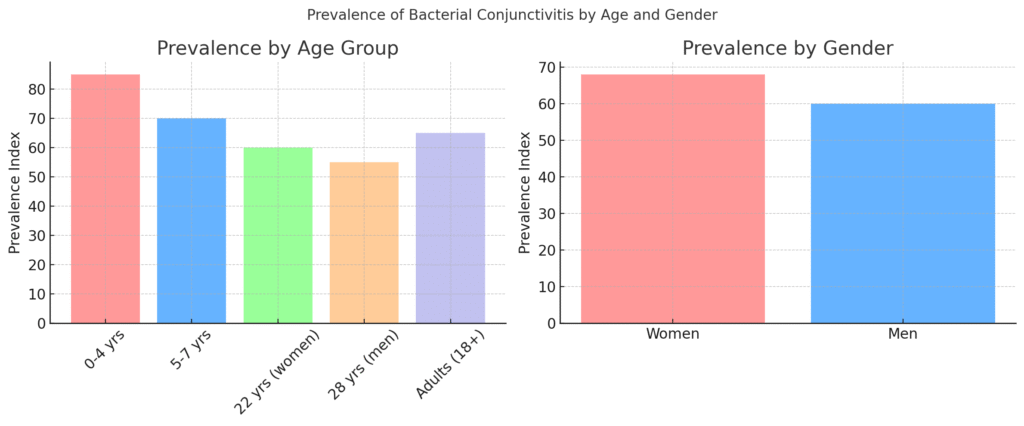
Adults: A secondary peak is seen in women around 22 years and men around 28 years (Review of Optometry, 2021).
Gender Differences
Women have a slightly higher prevalence of conjunctivitis than men
In adults aged 18+, women are more likely to develop conjunctivitis due to:
Possible reasons include contact lens use, occupational exposure, and hormonal influences.(Cureus ,2022)
Makeup and cosmetic products introducing bacteria (CDC, 2023).
4. Conjunctivitis Treatment & Medications
Bacterial Conjunctivitis Treatment & Medications
Treatment:
- Usually improves within 24–48 hours of starting antibiotic therapy
🧪 Medications:
- Topical Antibiotics (Eye Drops or Ointments):
- Tobramycin (Tobrex®) for Conjunctivitis (effective against Staphylococcus)
- Ciprofloxacin (Ciloxan®) drops (for severe cases)
- Erythromycin ophthalmic ointment (safe for kids)
- Ofloxacin (Floxin®)
- Trimethoprim/polymyxin B (Polytrim®)
- Besivance® (Besifloxacin) – newer generation fluoroquinolone
- Zymaxid® (Gatifloxacin)
👶 Newborns with bacterial conjunctivitis (e.g., from gonorrhea or chlamydia) require immediate systemic and topical treatment.
Viral Conjunctivitis Treatment & Medications
Treatment:
- Self-limiting – usually resolves on its own in 7–14 days
- No specific antiviral treatment for most viral causes (except for herpes-related cases)
🧪 Medications:
- Artificial tears (to soothe irritation)
- Cold compresses
- Antiviral drops if caused by herpes virus:
- Trifluridine (Viroptic®)
- Ganciclovir ophthalmic gel (Zirgan®)
- Oral Acyclovir , Valacyclovir , or Famciclovir may be prescribed for severe HSV/VZV cases
⚠️ No antibiotics are effective for typical viral conjunctivitis.
Allergic Conjunctivitis Treatment & Medications
Treatment:
- Avoid allergen exposure
- Cold compresses
- Lubricating eye drops
🧪 Medications:
- Mast cell stabilizers:
- Ketotifen fumarate (Zaditor®, Alaway®)
- Lodoxamide tromethamine (Alomide®)
- Antihistamine drops:
- Olopatadine (Patanol®, Pataday®)
- Epinastine (Elestat®)
- Pheniramine maleate/naphazoline HCl (Naphcon-A®, Opcon-A®)
- Dual-action antihistamine/mast cell stabilizers:
- Olopatadine
- Bepotastine besilate (Bepreve®)
- Azelastine (Optivar®)
- Steroid drops (short-term use only under supervision):
- Loteprednol etabonate (Alrex®, Lotemax®)
⚠️ Steroids should not be used long-term due to risk of glaucoma and cataracts.
Drug Interactions & Special Cases
Medication Interactions
Though topical treatments have low systemic absorption, there are noteworthy bacterial conjunctivitis medication interactions, especially when treating patients with:(Aziz Sheikh et al.2005)
- Anxiety : No Significant Drug Interactions Reported. Monitor for CNS effects.
- ADHD: Stimulants like amphetamines may dry the eye surface, potentially exacerbating irritation.
- Gout: Some antibiotics, particularly fluoroquinolones, may aggravate tendon inflammation.
- Diabetes: Slower healing increases the risk of prolonged conjunctivitis and secondary infections.
- UTI treatments: Concurrent systemic antibiotics may contribute to antimicrobial resistance.
- Osteoporosis: Bisphosphonates can inflame ocular tissue; monitor closely.
- Shingles: Requires systemic antivirals if ocular structures are involved, along with topical antibiotics.
- COVID-19: Immunosuppression may require more aggressive or prolonged therapy.
- Dementia/OCD: Polypharmacy increases risks of confusion and incorrect drop administration.
- Sinus Infections: Conjunctivitis with sinus infection often indicates broader upper respiratory tract involvement and may need systemic antibiotics.
- Depression meds? Unlikely to pose a risk .
- Diabetics? Steroid eye drops can raise blood sugar
C. Side Effects & Warnings
- Temporary blurred vision (common with ointments)
- Allergic reactions (stop use if swelling occurs)
5. Home Remedies & Alternative Treatments
Does Breast Milk Help Conjunctivitis?
Some believe breast milk for conjunctivitis works due to antibodies, but research is limited (BMJ, 2021). Risks include bacterial contamination.
Safe Home Care
- Cold compresses (reduce swelling)
- Artificial tears (lubricate dry eyes)
- Avoid touching eyes! (prevents reinfection)
6. Prevention
How Contagious Is Pink Eye?
- Bacterial conjunctivitis contagious period: 24-48 hrs after antibiotics (CDC).
FAQS Conjunctivitis (Pink Eye):
Can Kids Go to School?
Yes, after 24 hrs of antibiotics—but check school policies
Can You Wear Contacts?
No! Switch to glasses until healed.
Is pink eye contagious?
Yes! Bacterial/viral types spread easily.
Can breast milk cure pink eye?
No strong evidence—see a doctor instead









Good info. Lucky me I reach on your website by accident, I bookmarked it.