Table of Contents
Gout, a form of inflammatory arthritis, has plagued humanity for centuries. From ancient Greek physician Hippocrates to famous figures like Benjamin Franklin and King Henry VIII, this painful condition has left its mark on history.
Gout occurs when uric acid crystals accumulate in joints, leading to intense pain and inflammation. It’s a complex interplay of genetics, diet, and lifestyle factors.

Definition and Classification
Gout is a type of inflammatory arthritis characterized by the deposition of monosodium urate crystals in joints and surrounding tissues.
- It’s classified as a metabolic disorder, falling under the broader category of crystal-induced arthropathies.
The condition typically manifests in two forms: acute gout and chronic gout.
- Acute gout involves sudden, severe attacks of pain, swelling, and redness in joints.
- Chronic gout, on the other hand, develops over time with repeated flare-ups and can lead to joint damage if left untreated.
Gout is often confused with pseudogout, another form of crystal-induced arthritis. However, pseudogout is caused by calcium pyrophosphate crystals rather than uric acid crystals.
Prevalence and Risk Factors
Gout affects millions worldwide, with its prevalence increasing in recent decades.
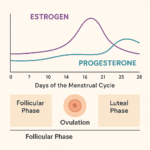
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), gout is more common in men, particularly those between 30 and 50 years old. Women typically develop gout after menopause.

Several risk factors contribute to the development of gout:
- Age and sex: Men are at higher risk, especially as they age.
- Genetics: Family history plays a role in gout susceptibility.
- Diet: Consumption of purine-rich foods and alcohol increases risk.
- Medical conditions: Obesity, hypertension, and diabetes are associated with higher gout risk.
- Medications: Certain drugs, like diuretics, can affect uric acid levels.
Understanding these risk factors is crucial for both prevention and management of gout. By identifying and addressing modifiable risk factors, individuals can take proactive steps to reduce their chances of developing this painful condition.
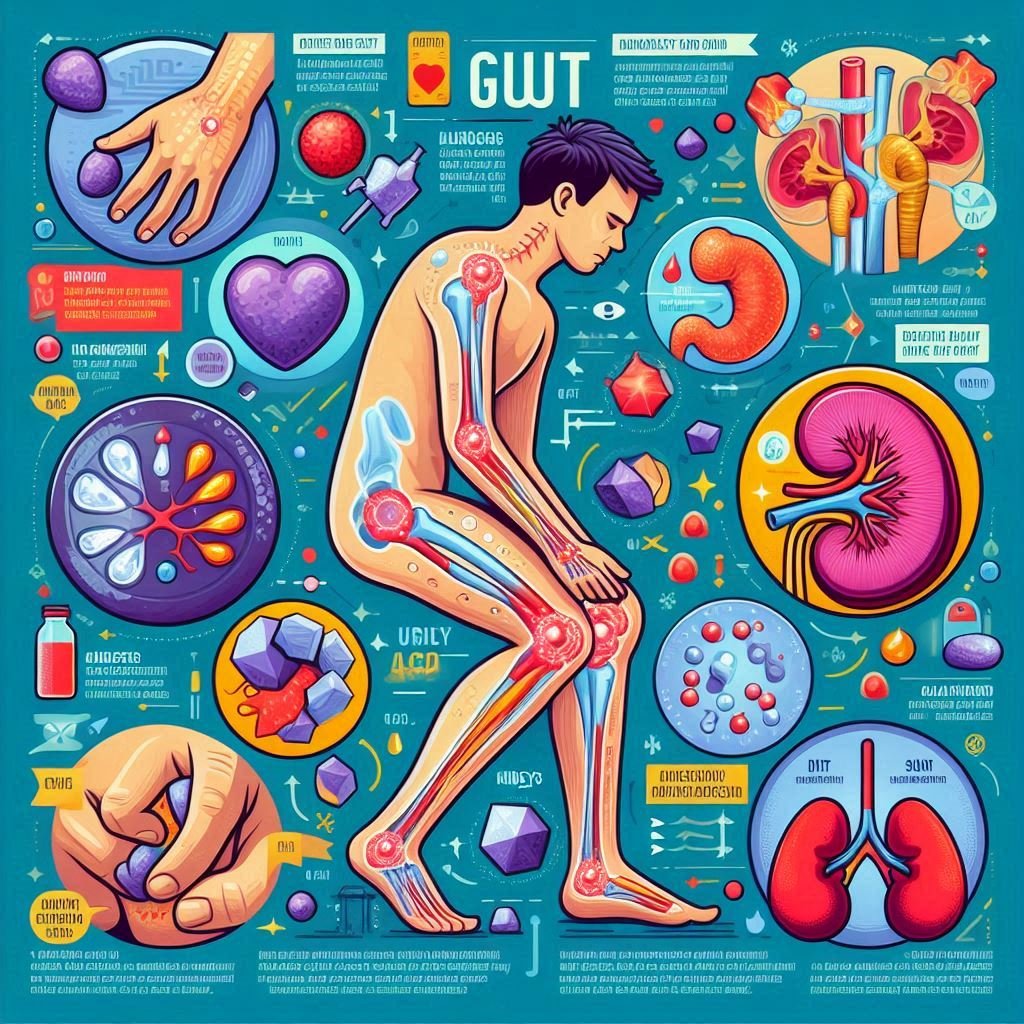
Symptoms of Gout
Gout symptoms can be as dramatic as they are painful. From the sudden onset of excruciating joint pain to visible changes in affected areas, gout makes its presence known in no uncertain terms. Let’s explore the various ways this condition manifests.
Acute Gout Attack Signs
An acute gout attack, also known as a gout flare-up, often strikes without warning. Here’s what you might experience:
- Intense joint pain: Usually starting in the big toe (a condition called podagra), the pain can be severe enough to wake you from sleep.
- Inflammation: The affected joint becomes swollen, red, and warm to the touch.
- Limited range of motion: As the joint swells, movement becomes difficult and painful.
- Skin changes: The skin over the affected joint may appear shiny and peel as the attack subsides.
These acute attacks typically reach their peak intensity within 12-24 hours and can last for days or even weeks without treatment. The American College of Rheumatology emphasizes the importance of prompt treatment to reduce the duration and severity of these attacks.
Chronic Gout Manifestations
While acute attacks are the hallmark of gout, chronic gout presents its own set of challenges:
- Tophi formation: These are visible deposits of uric acid crystals under the skin, often appearing as chalky lumps.
- Joint damage: Repeated attacks can lead to erosion of joint surfaces and deformities.
- Persistent discomfort: Even between acute attacks, individuals may experience low-level pain and stiffness.
- Reduced quality of life: Chronic gout can impact daily activities and overall well-being.
The Arthritis Foundation highlights that proper management of chronic gout is crucial to prevent long-term joint damage and disability.
Affected Joints and Areas
While gout is infamous for affecting the big toe, it can target various joints throughout the body:
- Feet and ankles: After the big toe, these are the most commonly affected areas.
- Knees: Gout in the knee can be particularly debilitating, affecting mobility.
- Elbows, wrists, and fingers: Upper extremity involvement is less common but can occur.
- Spine: Rarely, gout can affect the spine, causing back pain and other complications.
It’s worth noting that gout typically affects one joint at a time, especially in its early stages. However, as the condition progresses, multiple joints may be involved simultaneously.
Understanding these symptoms is crucial for early diagnosis and treatment. If you’re experiencing any of these signs, especially recurrent joint pain and swelling, it’s important to consult a healthcare professional. Early intervention can make a significant difference in managing gout and preventing long-term complications.
Causes of Gout
Gout is a complex condition with multiple contributing factors. Understanding its causes is crucial for both prevention and management. Let’s delve into the key factors that lead to the development of this painful form of arthritis.
Uric Acid Buildup
At the heart of gout lies uric acid, a byproduct of purine metabolism. Here’s how it plays a central role:
- Hyperuricemia: This condition occurs when there’s too much uric acid in the blood.
- Crystal formation: Excess uric acid can form needle-like crystals in joints and surrounding tissues.
- Inflammatory response: The body’s immune system reacts to these crystals, causing inflammation and pain.
Recent research published in Nature Reviews Rheumatology highlights the complex interplay between uric acid levels and gout development. It’s important to note that not everyone with high uric acid levels will develop gout, but it’s a significant risk factor.
Genetic Factors
Genetics play a crucial role in gout susceptibility:
- Inherited traits: Some people inherit genes that affect uric acid production or excretion.
- Family history: Having a close relative with gout increases your risk.
- Genetic variants: Specific gene mutations can affect uric acid transport in the kidneys.
A study in the New England Journal of Medicine identified several genetic loci associated with gout risk, underscoring the hereditary component of this condition.
Dietary Triggers
Diet significantly influences gout risk and flare-ups:
- Purine-rich foods: Red meat, organ meats, and certain seafoods can increase uric acid levels.
- Alcohol: Beer and spirits, in particular, are associated with higher gout risk.
- Fructose: High-fructose corn syrup, found in many processed foods, may contribute to gout.
The Arthritis Foundation recommends a balanced diet low in purines to help manage gout. However, it’s important to consult with a healthcare provider or dietitian for personalized advice.
Medical Conditions Associated with Gout
Several health conditions are linked to an increased risk of gout:
- Obesity: Excess body weight is associated with higher uric acid production.
- Metabolic syndrome: This cluster of conditions, including high blood pressure and abnormal cholesterol levels, often coexists with gout.
- Kidney disease: Impaired kidney function can affect uric acid excretion.
- Diabetes: This condition is often associated with gout, though the exact relationship is complex.
A review in the Lancet highlighted the intricate relationships between gout and these comorbidities, emphasizing the need for comprehensive management approaches.
Understanding these causes is crucial for developing effective prevention and treatment strategies. By addressing modifiable risk factors like diet and managing associated health conditions, individuals can take proactive steps to reduce their gout risk or manage existing gout more effectively.
Diagnosis and Treatment
Accurate diagnosis and appropriate treatment are crucial for managing gout effectively. From identifying the condition to implementing long-term management strategies, let’s explore the key aspects of gout diagnosis and treatment.
Diagnostic Methods
Diagnosing gout involves several approaches:
- Clinical assessment: A healthcare provider will evaluate symptoms and medical history.
- Joint fluid analysis: This is the gold standard for gout diagnosis, involving the extraction and examination of synovial fluid for urate crystals.
- Blood tests: These can measure uric acid levels, though it’s important to note that levels may be normal during an acute attack.
- Imaging tests: X-rays, ultrasounds, or dual-energy CT scans can help visualize joint damage or urate crystal deposits.
The American College of Rheumatology emphasizes the importance of accurate diagnosis, as gout can sometimes be mistaken for other forms of arthritis.
Medications for Gout Management
Several medications are used to manage gout:
- For acute attacks:
- Colchicine: An anti-inflammatory drug that can relieve pain and swelling.
- NSAIDs: These can help reduce inflammation during flare-ups.
- Corticosteroids: Used in severe cases or when other medications aren’t suitable.
- For long-term management:
- Allopurinol: A uric acid-lowering therapy that inhibits uric acid production.
- Febuxostat: Another urate-lowering medication, often used when allopurinol isn’t tolerated.
- Probenecid: Helps the kidneys eliminate uric acid more effectively.
Recent research published in The Lancet Rheumatology has explored new therapeutic targets for gout, offering hope for more effective treatments in the future.
Lifestyle Changes and Prevention Strategies
Managing gout goes beyond medication. Lifestyle modifications play a crucial role:
- Dietary changes: Limiting purine-rich foods and alcohol intake can help reduce gout risk.
- Weight management: Maintaining a healthy weight can lower uric acid levels.
- Hydration: Drinking plenty of water helps flush out uric acid.
- Exercise: Regular physical activity can help manage weight and improve overall health.
The Arthritis Foundation provides comprehensive resources on lifestyle modifications for gout management, emphasizing the importance of a holistic approach.
Implementing these diagnostic and treatment strategies requires a collaborative effort between patients and healthcare providers. Regular follow-ups and adjustments to the treatment plan are often necessary to achieve optimal gout management.
Living with Gout
Managing gout is a lifelong journey that extends beyond medical treatments. It involves adapting your lifestyle, being mindful of your diet, and developing strategies to cope with flare-ups. Let’s explore how to navigate life with gout effectively.
Long-term Management
Living with gout requires a comprehensive, long-term approach:
- Regular check-ups: Monitoring uric acid levels and adjusting treatments as needed.
- Medication adherence: Consistently taking prescribed medications, even when symptom-free.
- Self-monitoring: Keeping track of potential triggers and early signs of flare-ups.
- Educating yourself: Staying informed about the latest gout research and management strategies.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) emphasizes the importance of partnering with healthcare providers for effective long-term gout management.
Diet and Nutrition Tips
Diet plays a crucial role in managing gout:
- Low-purine diet: Limiting high-purine foods like red meat, organ meats, and certain seafoods.
- Hydration: Drinking plenty of water to help flush out uric acid.
- Cherries: Some studies suggest cherries may help reduce gout flare-ups.
- Vitamin C: Moderate intake may help lower uric acid levels.
- Limit alcohol: Especially beer and spirits, which are associated with increased gout risk.
Remember, dietary changes should be made in consultation with a healthcare provider or registered dietitian to ensure nutritional needs are met.
Coping Strategies for Flare-ups
Despite best efforts, gout flare-ups can still occur. Here are some coping strategies:
- Rest and elevate: Keep the affected joint elevated and avoid putting pressure on it.
- Cold therapy: Applying ice packs can help reduce inflammation and pain.
- Pain management: Use prescribed medications as directed by your healthcare provider.
- Stress reduction: Practice relaxation techniques, as stress can exacerbate gout symptoms.
- Support network: Connect with friends, family, or support groups for emotional support.
The Arthritis Foundation offers resources and support groups for individuals living with gout, providing a valuable network for sharing experiences and coping strategies.
Living with gout requires patience, persistence, and a proactive approach to health. By implementing these strategies and working closely with healthcare providers, individuals with gout can minimize flare-ups, reduce long-term joint damage, and maintain a good quality of life.
Remember, everyone’s experience with gout is unique. What works for one person may not work for another, so it’s important to develop a personalized management plan in collaboration with your healthcare team.
FAQ for Gout Symptoms and Causes
What is the main cause of gout?
What is the best treatment for gout?
What foods cause gout?
Red meat (beef, lamb, and pork)
Organ meats (liver, kidney)
Seafood (anchovies, sardines, mussels, scallops)
Alcoholic beverages (especially beer and spirits)
Sugary drinks and foods high in fructose (such as soft drinks)
Limiting or avoiding these foods can help manage uric acid levels.
What are the first symptoms of uric acid?
Is egg good for uric acid?
What fruit is good for gout?
Cherries: Known for their ability to reduce uric acid levels and inflammation.
Citrus fruits: Oranges, lemons, and grapefruits are high in vitamin C, which can help lower uric acid levels.
Berries: Strawberries, blueberries, and blackberries have antioxidants that may reduce inflammation.
Apples and pears: These fruits have moderate amounts of fructose, making them safer choices in moderation.









fantastic post.Ne’er knew this, regards for letting me know.