Epilepsy is a neurological disorder that affects many women of childbearing age. When you’re pregnant and have epilepsy, you’re embarking on what’s considered a high-risk pregnancy. But don’t let that term scare you! It simply means you’ll need a bit more care and attention throughout your journey of Epilepsy and Pregnancy .
Table of Contents

The key to a healthy pregnancy with epilepsy? Planning, planning, and more planning!
Why is planning so important?
- It helps manage seizure risks during pregnancy
- It allows for medication adjustments before conception
- It ensures you’re getting the right prenatal care from the start
Preconception Planning of Epilepsy and pregnancy: Your First Step to a Healthy Pregnancy
Before you start trying for a baby, it’s crucial to have a chat with your neurologist and obstetrician. Think of it as assembling your dream team for this exciting journey!
During these preconception counselling sessions, you’ll discuss:
- Your current seizure management
- Any potential medication changes
- Genetic counselling options
- The importance of folic acid supplementation
Medication Review: Finding the Right Balance
One of the biggest concerns for women with epilepsy is how their antiepileptic drugs (AEDs) might affect their baby. Your neurologist will review your current meds and may suggest some changes.
For example, Lamotrigine is often considered a safer option for pregnancy. But remember, every woman is different, and what works for one might not work for another.
Top tip: Never stop or change your meds without talking to your doctor first!
Folic Acid: Your New Best Friend
All pregnant women need folic acid, but for women with epilepsy, it’s even more crucial. Why? Some AEDs can interfere with folic acid metabolism, potentially increasing the risk of certain birth defects.
Your doctor will likely recommend a higher dose of folic acid than what’s typically suggested for pregnant women. Start taking it before you conceive and continue throughout your pregnancy.
Managing Epilepsy During Pregnancy: Keeping You and Your Baby Safe
Once you’re pregnant, managing your epilepsy becomes a delicate balancing act. The goal is to control your seizures while minimising any risks to your developing baby.
Seizure Management Strategies
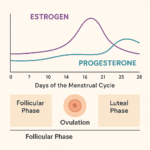
Pregnancy can be a bit of a rollercoaster for your body, and those hormonal changes can sometimes affect your seizure frequency. Some women find their seizures improve during pregnancy, while others might experience more frequent seizures.
Here are some strategies to help manage your seizures:
- Stick to a regular sleep schedule
- Avoid known seizure triggers
- Take your medications as prescribed
- Attend all your check-ups
Remember, having a seizure during pregnancy can be dangerous for both you and your baby. If you experience any changes in your seizure pattern, contact your healthcare team right away.
Medication Safety and Monitoring
Throughout your pregnancy, your neurologist will closely monitor your medication levels. This is because pregnancy can affect how your body processes AEDs.
You might need more frequent blood tests to check your medication levels. Don’t worry – this is all part of ensuring you’re getting the right dose to keep your seizures under control.
Alternative Treatments: Vagus Nerve Stimulation
For some women, vagus nerve stimulation (VNS) might be an option to help control seizures during pregnancy. This involves a small device implanted under the skin that sends electrical signals to the brain.
If you’re already using VNS, you can generally continue using it during pregnancy. However, always discuss this with your healthcare team.
Potential Risks to Fetal Development: What You Need to Know
It’s natural to worry about how epilepsy and its treatment might affect your baby. While there are some risks, remember that with proper care, most women with epilepsy have healthy pregnancies and babies.
Teratogenic Effects of Antiepileptic Drugs
Some AEDs can have teratogenic effects, meaning they might cause birth defects. The risks vary depending on the specific medication and dosage.
Common concerns include:
- Neural tube defects
- Cleft lip or palate
- Heart defects
- Developmental delays
However, it’s important to balance these risks against the risks of uncontrolled seizures during pregnancy. Your healthcare team will help you make the best decision for your situation.
Minimising Risks Through Proper Care
While we can’t eliminate all risks, there’s a lot we can do to minimise them:
- Take folic acid supplements
- Attend all prenatal check-ups
- Follow your medication regimen as prescribed
- Avoid alcohol and smoking
- Eat a healthy, balanced diet
Remember, many of these risks are relatively small, and most women with epilepsy have healthy babies. Stay positive and focus on taking good care of yourself!
Comprehensive Prenatal Care: Extra TLC for You and Your Baby
When you’re pregnant with epilepsy, you’ll likely have more frequent prenatal check-ups. This extra monitoring helps ensure that both you and your baby are doing well.
Frequent Check-ups and Monitoring
Your prenatal care might include:
- Regular ultrasounds to check your baby’s development
- More frequent blood tests to monitor your AED levels
- Check-ups with both your obstetrician and neurologist
Don’t be surprised if you’re seeing your doctors more often than your pregnant friends without epilepsy. This extra care is all about keeping you and your baby healthy!
Obstetric Care for High-Risk Pregnancies
Your pregnancy will be managed as a high-risk pregnancy. This doesn’t mean something will go wrong – it just means you’ll get some extra attention and care.
Your obstetric team will be experienced in managing high-risk pregnancies and will work closely with your neurologist to provide comprehensive care.
Fetal Development Monitoring
Your healthcare team will keep a close eye on your baby’s development throughout your pregnancy. This might include:
- Detailed ultrasounds to check for any structural abnormalities
- Fetal echocardiograms to check your baby’s heart
- Non-invasive prenatal testing (NIPT) for genetic conditions
Remember, most of these tests are precautionary. Try not to worry too much if you’re asked to have extra screenings – it’s all part of ensuring the best care for you and your baby.
Labour and Delivery: Preparing for Your Big Day with epilepsy and pregnancy
As your due date approaches, it’s time to start thinking about your birth plan. Having epilepsy doesn’t mean you can’t have the birth experience you want, but there are a few extra considerations to keep in mind.
Creating Your Birth Plan
When creating your birth plan, consider:
- Your preferred pain relief options
- Who you want present during labour
- Your preferences for managing potential seizures during labour
- Your thoughts on breastfeeding
Discuss your birth plan with your healthcare team. They can help you understand what to expect and how to prepare for different scenarios.
Managing Seizure Risks During Labour
Labour can be physically and emotionally stressful, which could potentially trigger a seizure. To minimise this risk:
- Ensure you take your AEDs as usual during labour
- Try to get as much rest as possible in early labour
- Use relaxation techniques to stay calm
- Inform the delivery team about your epilepsy and any specific instructions from your neurologist
Remember, the delivery team will be prepared to manage any seizures that might occur during labour. Your safety and your baby’s safety are their top priority.
Coordinating Care Between Neurology and Obstetrics
Your neurologist and obstetrician will work together to ensure you have the safest possible delivery. They’ll coordinate your care and be available to handle any epilepsy-related issues that might arise during labour and delivery.
Don’t be shy about asking questions or expressing your concerns. Your healthcare team is there to support you every step of the way!
FAQ for epilepsy and pregnancy
Can epilepsy complicate pregnancy?
Increased risk of seizures: Hormonal changes and sleep disturbances during pregnancy can trigger seizures.
Effects of anti-seizure medications: Certain anti-epileptic drugs (AEDs) may pose risks to the developing baby, including congenital malformations. However, uncontrolled seizures may also pose a risk, so balancing medication is crucial.
Increased monitoring: Pregnant women with epilepsy often require more frequent check-ups and adjustments to their treatment plan.
How to manage epilepsy during pregnancy?
Pre-conception planning: If you’re planning to get pregnant, consult your healthcare provider to adjust medications and ensure your condition is well-controlled before conceiving.
Medication adjustments: Some anti-seizure medications may need to be adjusted to minimize risks to the baby. Your doctor will try to prescribe the lowest effective dose to control seizures while minimizing harm.
Folic acid supplementation: Women with epilepsy are often advised to take a higher dose of folic acid (4-5 mg per day) before and during pregnancy to reduce the risk of neural tube defects, which can be increased by certain anti-seizure medications.
Frequent check-ups: Regular visits to both a neurologist and an obstetrician are essential. Blood levels of medications may be monitored to ensure that they remain therapeutic as pregnancy progresses.
Lifestyle management: Prioritize good sleep, a healthy diet, and stress reduction, as these factors can influence seizure control.
Seizure action plan: Work with your doctor to create an action plan in case of a seizure during pregnancy. This includes knowing when to seek emergency care and how to manage seizures safely.
What happens when a pregnant woman has a seizure?
Impact on the baby: Seizures can reduce the amount of oxygen reaching the baby, which may increase the risk of developmental issues, preterm labor, or low birth weight.
Physical injury: Tonic-clonic (grand mal) seizures pose a risk of injury to the mother due to falls or trauma, which can indirectly affect the baby.
Increased risks with prolonged seizures: If seizures are frequent or prolonged (status epilepticus), there is a higher risk of complications for both the mother and baby, requiring emergency care.s knowing when to seek emergency care and how to manage seizures safely.
Should you have a baby if you have epilepsy?
Pre-pregnancy consultation: It’s important to work with your healthcare provider to plan the best time for pregnancy when your epilepsy is well-controlled.
Risk assessment: Discuss with your doctor the potential risks and benefits of continuing or adjusting your anti-seizure medications during pregnancy.
Genetic counseling: There is a slightly higher risk of epilepsy being passed on to the child, so you may want to meet with a genetic counselor to discuss this.
Support system: Having a strong support system is essential, as stress and lack of sleep can trigger seizures. Family or professional support can help ensure a smoother pregnancy.
Will my child inherit epilepsy if I have it?
Are there special precautions for delivery if I have epilepsy?
Medication adjustments: Your doctor will adjust your medications, if necessary, close to your due date to prevent seizures during labor.
Hospital delivery: It’s recommended that women with epilepsy give birth in a hospital where specialized care is available if needed.
Postpartum care: After delivery, seizure frequency can increase due to hormonal shifts and sleep deprivation, so close monitoring and support are important.









2 thoughts on “Epilepsy and Pregnancy: Essential Tips for a Safe and Healthy Journey”