
Table of Contents
What are GLP-1 Drugs/Medications
GLP-1 drugs/medications have revolutionized the treatment landscape for both type 2 diabetes and obesity. These innovative pharmaceuticals, known as glucagon-like peptide-1 receptor agonists (GLP-1 RAs), have gained significant attention not only for their effectiveness in managing blood glucose levels but also for their remarkable weight loss benefits.
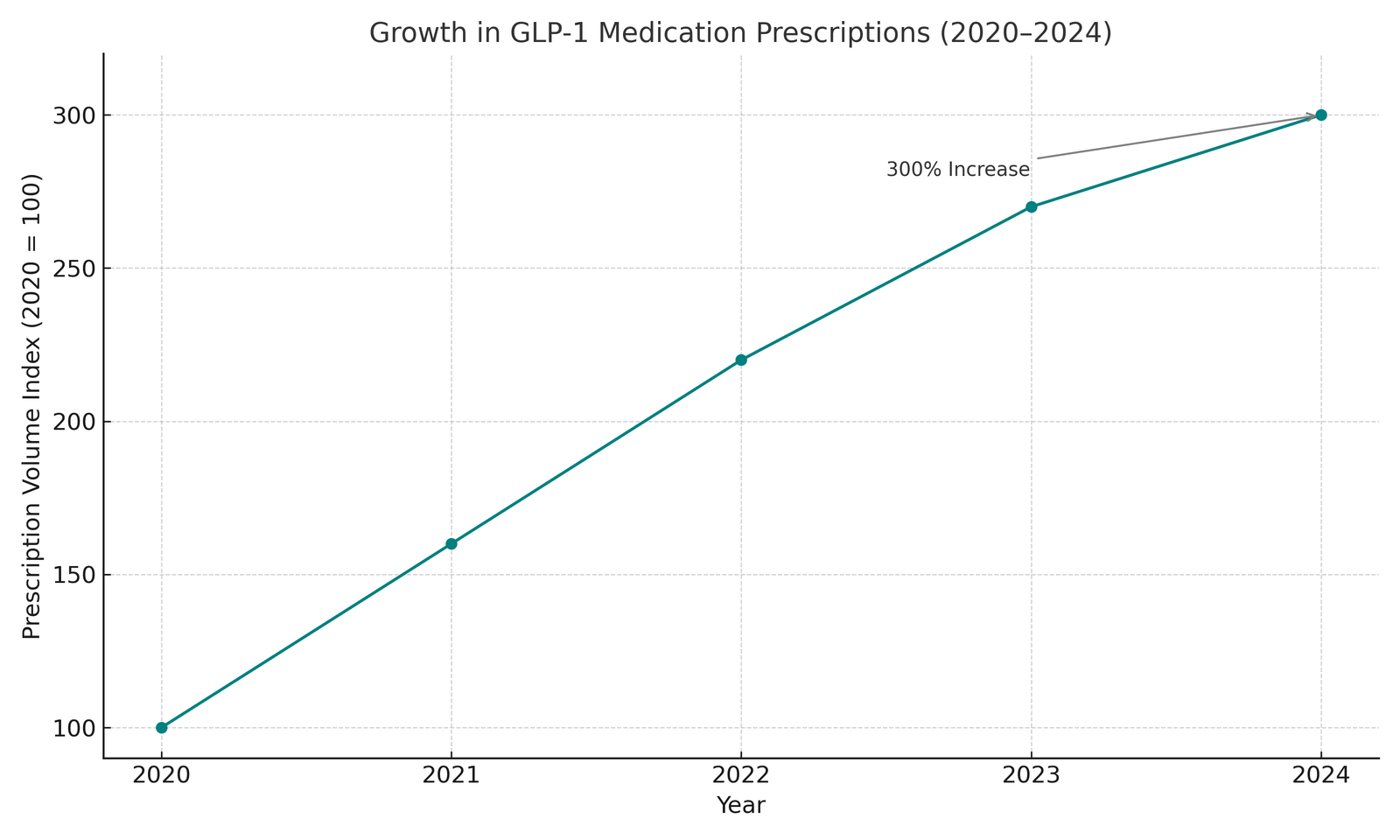
- The popularity of GLP-1 medications has surged dramatically in recent years.
- According to the American Diabetes Association’s 2025 Standards of Care, prescriptions for GLP-1 medications increased by over 300% between 2020 and 2024.
- This exponential growth reflects both their clinical effectiveness and the growing awareness among healthcare providers and patients about their benefits beyond diabetes management.
.
How GLP-1 Medications Work
GLP-1 medications work by mimicking the action of a naturally occurring hormone in your body called glucagon-like peptide-1. This hormone plays several crucial roles in regulating blood glucose and appetite. Understanding the mechanism of action helps explain why these medications are effective for both diabetes management and weight loss.
The Science Behind GLP-1
When you eat, your intestines naturally release GLP-1, which triggers several important physiological responses:
- Insulin secretion: GLP-1 stimulates the pancreas to release insulin in response to rising blood glucose levels, but only when blood sugar is elevated. This “glucose-dependent” action is what makes GLP-1 medications less likely to cause hypoglycemia (low blood sugar) compared to some other diabetes treatments.
- Glucagon suppression: GLP-1 inhibits the release of glucagon, a hormone that raises blood glucose levels. By reducing glucagon secretion, GLP-1 helps prevent the liver from releasing excess glucose into the bloodstream.
- Delayed gastric emptying: GLP-1 slows the rate at which food leaves your stomach and enters your small intestine. This delayed gastric emptying helps prevent rapid spikes in blood sugar after meals and contributes to feelings of fullness.
- Appetite regulation: GLP-1 acts on the brain’s appetite center, specifically the hypothalamus, reducing hunger signals and increasing satiety. This effect is particularly important for the weight loss benefits of these medications.
GLP-1 Medications vs. Natural GLP-1
Natural GLP-1 has a very short half-life in the body – it’s broken down within minutes by an enzyme called dipeptidyl peptidase-4 (DPP-4). GLP-1 medications are designed to resist this breakdown, allowing them to remain active in the body for hours or even days, depending on the specific formulation. This extended action is what makes them effective as therapeutic agents.
According to research published in the New England Journal of Medicine (2024), GLP-1 medications can increase active GLP-1 levels in the bloodstream by 3-5 times compared to natural levels, enhancing and prolonging the beneficial effects of this hormone.
Types of GLP-1 Medications
There are several GLP-1 medications available on the market, each with unique characteristics regarding dosing frequency, administration method, and approved indications. Here’s a comprehensive overview of the major GLP-1 medications currently available:
Short-Acting GLP-1 Receptor Agonists
1. Exenatide (Byetta)
- Administration: Twice-daily injection
- Approved for: Type 2 diabetes
- Unique features: The first GLP-1 RA approved by the FDA (2005)
- Typical starting dose: 5 mcg twice daily, can be increased to 10 mcg twice daily
2. Lixisenatide (Adlyxin)
- Administration: Once-daily injection
- Approved for: Type 2 diabetes
- Unique features: Particularly effective at reducing post-meal glucose spikes
- Typical starting dose: 10 mcg once daily for 14 days, then increased to 20 mcg once daily
Long-Acting GLP-1 Receptor Agonists
3. Exenatide extended-release (Bydureon)
- Administration: Once-weekly injection
- Approved for: Type 2 diabetes
- Unique features: Uses microsphere technology to slowly release the medication
- Typical starting dose: 2 mg once weekly
4. Dulaglutide (Trulicity)
- Administration: Once-weekly injection
- Approved for: Type 2 diabetes
- Unique features: Comes in a single-use pen that doesn’t require needle handling
- Typical starting dose: 0.75 mg once weekly, can be increased to 1.5 mg, 3 mg, or 4.5 mg
5. Semaglutide (Ozempic, Wegovy, Rybelsus)
- Administration:
- Ozempic: Once-weekly injection for diabetes
- Wegovy: Once-weekly injection for weight management
- Rybelsus: Once-daily oral tablet (the only oral GLP-1 RA)
- Approved for:
- Ozempic: Type 2 diabetes
- Wegovy: Weight management
- Rybelsus: Type 2 diabetes
- Unique features: Highest weight loss efficacy among GLP-1 RAs; Rybelsus is the first oral GLP-1 medication
- Typical starting dose:
- Ozempic: 0.25 mg once weekly for 4 weeks, then 0.5 mg once weekly
- Wegovy: Gradual titration from 0.25 mg to 2.4 mg once weekly over 16+ weeks
- Rybelsus: 3 mg once daily for 30 days, then 7 mg once daily
6. Tirzepatide (Mounjaro, Zepbound)
- Administration: Once-weekly injection
- Approved for:
- Mounjaro: Type 2 diabetes
- Zepbound: Weight management
- Unique features: Dual GIP/GLP-1 receptor agonist (not purely a GLP-1 RA, but often grouped with them)
- Typical starting dose: 2.5 mg once weekly, with gradual titration up to 15 mg
Combination Products
7. Insulin glargine/Lixisenatide (Soliqua)
- Administration: Once-daily injection
- Approved for: Type 2 diabetes
- Unique features: Combines a long-acting insulin with a GLP-1 RA
- Typical starting dose: Based on previous insulin dose or 15 units/5 mcg once daily
8. Insulin degludec/Liraglutide (Xultophy)
- Administration: Once-daily injection
- Approved for: Type 2 diabetes
- Unique features: Combines a long-acting insulin with a GLP-1 RA
- Typical starting dose: 10 units/0.36 mg once daily
According to the American Diabetes Association’s 2025 guidelines, semaglutide and tirzepatide currently show the strongest evidence for both glycemic control and weight reduction among the available options. However, the best choice depends on individual patient factors, including insurance coverage, injection preference, and specific health goals.
GLP-1 Medications for Diabetes
GLP-1 receptor agonists have become cornerstone treatments for type 2 diabetes, offering multiple benefits beyond simple glucose control. Here’s what makes them particularly valuable in diabetes management:
Glycemic Benefits
Clinical studies published in The Lancet Diabetes & Endocrinology (2024) demonstrate that GLP-1 medications can reduce hemoglobin A1C (a three-month average of blood glucose levels) by 1.0-1.8 percentage points on average. This reduction is clinically significant and often superior to many other diabetes medications.
The glucose-lowering effects of GLP-1 medications are particularly notable because:
- They primarily work when blood glucose is elevated, reducing the risk of hypoglycemia
- They help control both fasting and post-meal glucose levels
- Their efficacy doesn’t diminish significantly over time, unlike some other diabetes medications
Cardiovascular Benefits
Perhaps one of the most important advantages of certain GLP-1 medications is their proven cardiovascular benefit. Large-scale clinical trials have demonstrated that some GLP-1 RAs (specifically semaglutide, dulaglutide, and liraglutide) can reduce the risk of major adverse cardiovascular events (MACE) in people with type 2 diabetes who have established cardiovascular disease or are at high risk.

The PIONEER 6 trial, published in the New England Journal of Medicine, showed that semaglutide reduced the risk of cardiovascular death, non-fatal heart attack, or non-fatal stroke by 21% compared to placebo. Similar benefits have been observed with other GLP-1 medications, leading the American Diabetes Association and American College of Cardiology to recommend GLP-1 RAs as preferred second-line agents after metformin for patients with established cardiovascular disease.
Renal Protection
Emerging evidence suggests that GLP-1 medications may also offer kidney protection for people with type 2 diabetes. The AWARD-7 trial demonstrated that dulaglutide slowed the decline in estimated glomerular filtration rate (eGFR), a measure of kidney function, compared to insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease.
Where GLP-1s Fit in Diabetes Treatment Guidelines
According to the 2025 American Diabetes Association Standards of Care, GLP-1 receptor agonists are recommended as:
- Second-line therapy after metformin for most patients with type 2 diabetes
- First-line therapy for patients with type 2 diabetes and established cardiovascular disease
- Preferred agents for patients who need to minimize hypoglycemia
- Preferred agents for patients who would benefit from weight loss
The European Association for the Study of Diabetes (EASD) offers similar recommendations, highlighting the importance of these medications in modern diabetes management.
which GLP-1 medications are approved for weight loss
While initially developed for diabetes treatment, the significant weight loss effects of GLP-1 medications have led to specific approvals for weight management. This section explores their role in treating obesity and overweight conditions.
FDA-Approved GLP-1s for Weight Management
Currently, two GLP-1 receptor agonists are specifically approved by the FDA for chronic weight management:
- Semaglutide (Wegovy): Approved in 2021 at a higher dose (2.4 mg weekly) than the diabetes formulation (Ozempic)
- Tirzepatide (Zepbound): Approved in 2023, with doses ranging from 2.5 mg to 15 mg weekly
These medications are indicated for:
- Adults with a BMI ≥30 kg/m² (obesity), or
- Adults with a BMI ≥27 kg/m² (overweight) with at least one weight-related comorbidity (such as hypertension, type 2 diabetes, or dyslipidemia)
Effectiveness for Weight Loss
The weight loss results from GLP-1 medications have been unprecedented in the pharmaceutical treatment of obesity:
- Semaglutide (Wegovy): The STEP-1 trial published in the New England Journal of Medicine showed that participants lost an average of 14.9% of their body weight after 68 weeks, compared to 2.4% with placebo.
- Tirzepatide (Zepbound): The SURMOUNT-1 trial demonstrated even more impressive results, with participants losing an average of 20.9% of their body weight at the highest dose (15 mg) after 72 weeks.
These results surpass the efficacy of all previous anti-obesity medications and approach the weight loss typically seen with bariatric surgery, though through a less invasive approach.

Mechanism of Weight Loss
GLP-1 medications promote weight loss through several mechanisms:
- Appetite suppression: They act on receptors in the brain’s hypothalamus to reduce hunger signals and increase feelings of fullness.
- Delayed gastric emptying: By slowing the movement of food from the stomach to the small intestine, they prolong the sensation of fullness after meals.
- Food preference changes: Some research suggests that GLP-1 medications may reduce cravings for high-fat and high-sugar foods, though this effect requires further study.
- Increased energy expenditure: Limited evidence suggests these medications might slightly increase caloric burn, though this is not considered their primary mechanism.
According to research published in Cell Metabolism (2024), the appetite-suppressing effects account for approximately 80% of the weight loss seen with these medications, with the remaining effects attributed to other mechanisms.
Long-Term Use for Weight Management
An important consideration with GLP-1 medications for weight management is that they typically require long-term, possibly indefinite use to maintain weight loss. The STEP-4 trial demonstrated that when semaglutide was discontinued after 68 weeks, participants regained approximately two-thirds of their lost weight within the following year.
This finding aligns with our understanding of obesity as a chronic disease requiring ongoing management, similar to how hypertension or diabetes typically require continuous treatment. Patients considering these medications should understand that they represent a long-term commitment rather than a short-term solution.
Side Effects and Safety Considerations
While GLP-1 medications offer significant benefits, they also come with potential side effects and safety considerations that patients and healthcare providers should carefully evaluate.
Common Side Effects
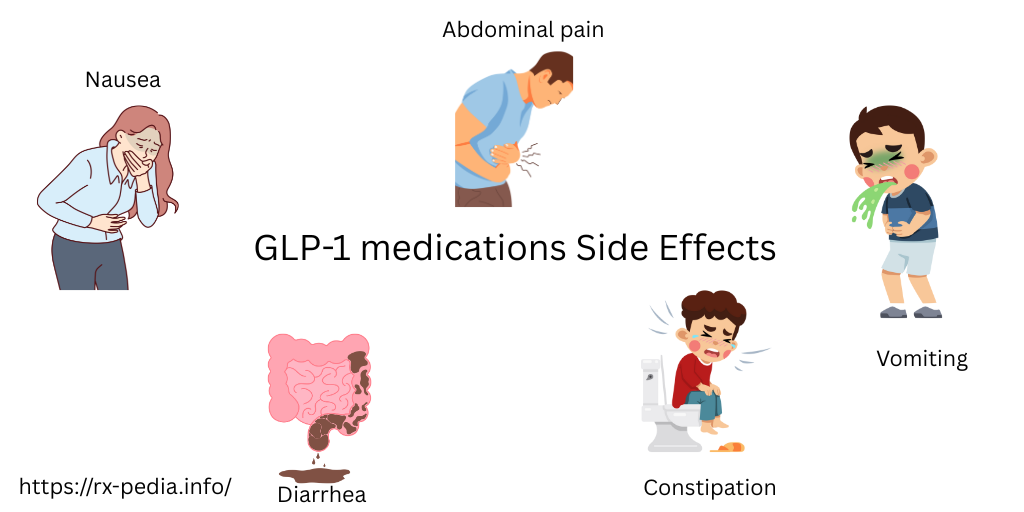
The most frequently reported side effects of GLP-1 medications involve the gastrointestinal system:
- Nausea: Affects approximately 30-40% of patients, typically most pronounced when starting the medication or increasing the dose
- Vomiting: Occurs in about 15-25% of patients
- Diarrhea: Reported by roughly 10-20% of patients
- Constipation: Experienced by approximately 10-15% of patients
- Abdominal pain: Affects about 10-15% of patients
These side effects are generally mild to moderate in severity and tend to diminish over time as the body adjusts to the medication. According to a meta-analysis published in JAMA Internal Medicine (2024), approximately 5-10% of patients discontinue GLP-1 medications due to gastrointestinal side effects.
Strategies to Minimize Side Effects
Several approaches can help reduce the likelihood and severity of gastrointestinal side effects:
- Gradual dose titration: Starting with a lower dose and gradually increasing it over weeks or months allows the body to adjust and typically reduces side effects.
- Dietary modifications: Smaller, more frequent meals and avoiding high-fat foods can help minimize nausea and other digestive symptoms.
- Adequate hydration: Drinking plenty of water can help manage constipation, a common side effect.
- Timing of meals: Some patients find that certain meal timing strategies (such as eating more earlier in the day) can help manage side effects.
- Anti-nausea medications: In some cases, healthcare providers may prescribe anti-nausea medications for short-term use during the initial adjustment period.
Serious Safety Concerns
While less common, there are several more serious safety concerns associated with GLP-1 medications that require attention:
Pancreatitis
GLP-1 medications carry a warning about acute pancreatitis (inflammation of the pancreas). While rare, occurring in less than 0.3% of patients according to post-marketing data, pancreatitis can be serious. Patients should be aware of symptoms such as severe abdominal pain that may radiate to the back, sometimes accompanied by vomiting, and seek immediate medical attention if these occur.
Thyroid C-Cell Tumors
Based on animal studies, GLP-1 medications carry a boxed warning about the risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC). This risk has not been confirmed in humans, but these medications are contraindicated in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Gallbladder Disease
Rapid weight loss from any cause, including GLP-1 medications, can increase the risk of gallstones. Clinical trials have shown a higher incidence of gallbladder-related issues (such as cholelithiasis and cholecystitis) in patients taking GLP-1 medications compared to placebo.
Acute Kidney Injury
Dehydration from gastrointestinal side effects can potentially lead to acute kidney injury. Patients with pre-existing kidney disease should be monitored closely, and all patients should maintain adequate hydration.
Diabetic Retinopathy Complications
In patients with type 2 diabetes and pre-existing diabetic retinopathy, rapid improvement in blood glucose control with any treatment, including GLP-1 medications, may be associated with temporary worsening of retinopathy. Regular eye examinations are recommended.
Special Populations
Pregnancy and Breastfeeding
GLP-1 medications are not recommended during pregnancy unless the potential benefit justifies the potential risk to the fetus. There is limited data on their use during breastfeeding. Women of childbearing age should use effective contraception while taking these medications.
Elderly Patients
Older adults may be more sensitive to the effects of GLP-1 medications, particularly the gastrointestinal side effects. Careful monitoring and potentially slower dose titration may be necessary.
Children and Adolescents
As of 2025, semaglutide (Wegovy) is the only GLP-1 medication approved for weight management in adolescents aged 12 years and older with obesity. Safety and efficacy data in pediatric populations are still limited compared to adults.
Cost and Insurance Coverage
The cost of GLP-1 medications represents a significant consideration for many patients, as these medications tend to be expensive compared to older diabetes and weight management treatments.
Retail Pricing
Without insurance or other forms of assistance, the retail prices of GLP-1 medications in the United States are substantial:
- Semaglutide (Ozempic/Wegovy): Approximately $900-$1,300 per month
- Tirzepatide (Mounjaro/Zepbound): Approximately $1,000-$1,400 per month
- Dulaglutide (Trulicity): Approximately $800-$1,100 per month
- Liraglutide (Victoza/Saxenda): Approximately $850-$1,200 per month
These prices reflect 2025 average retail costs and may vary by pharmacy and location.
Insurance Coverage
Insurance coverage for GLP-1 medications varies significantly:
For Diabetes Treatment
Most insurance plans, including Medicare Part D and Medicaid in many states, provide coverage for GLP-1 medications when prescribed for type 2 diabetes. However, many plans require prior authorization, meaning the healthcare provider must document that the patient meets specific criteria, which may include:
- Failure to achieve adequate control with metformin or other first-line medications
- Specific A1C thresholds (often >7% or >7.5%)
- Documentation of other factors such as cardiovascular disease or need for weight loss
For Weight Management
Coverage for GLP-1 medications prescribed specifically for weight management (Wegovy, Zepbound, Saxenda) is much more limited:
- Many private insurance plans exclude weight loss medications from coverage
- Medicare specifically excludes coverage for medications used for weight loss
- Some employer-sponsored plans have begun adding coverage, recognizing the long-term health benefits and potential cost savings
According to a 2025 survey by the Obesity Medicine Association, approximately 30% of private insurance plans offer some coverage for anti-obesity medications, though often with significant restrictions and high patient cost-sharing.
Patient Assistance Programs
Pharmaceutical manufacturers offer various assistance programs:
- Manufacturer savings cards: For commercially insured patients, these can reduce out-of-pocket costs significantly, sometimes to as little as $25-$100 per month
- Patient assistance programs: For uninsured or underinsured patients who meet income qualifications, these programs may provide medications at no cost
- Bridge programs: Some manufacturers offer free medication for a limited time while patients work through insurance approval processes
Cost-Effectiveness Considerations
Despite their high upfront cost, several analyses suggest GLP-1 medications may be cost-effective in the long term due to:
- Reduced complications from diabetes
- Decreased cardiovascular events
- Fewer hospitalizations
- Improvements in obesity-related conditions
- Potential reductions in other medication needs
A 2025 analysis published in JAMA Network Open estimated that treatment with semaglutide for weight management becomes cost-effective after approximately 7-10 years when considering the reduced healthcare costs associated with obesity-related conditions.
Lifestyle Considerations
While GLP-1 medications can be powerful tools for managing diabetes and weight, they work best when combined with appropriate lifestyle modifications. This section explores how to optimize the benefits of these medications through diet, exercise, and other lifestyle factors.
Dietary Recommendations
GLP-1 medications often change how patients experience hunger and fullness, creating an opportunity to establish healthier eating patterns. Optimal dietary approaches include:
Portion Control
Many patients on GLP-1 medications report feeling satisfied with smaller portions. Recommendations include:
- Using smaller plates and bowls
- Eating slowly and mindfully
- Stopping when comfortably full, not completely full
- Avoiding “cleaning your plate” out of habit
Food Quality
The quality of food becomes increasingly important when eating less overall:
- Prioritize nutrient-dense foods (vegetables, fruits, lean proteins, whole grains)
- Ensure adequate protein intake (0.8-1.2g per kg of body weight) to preserve muscle mass during weight loss
- Include healthy fats from sources like olive oil, avocados, and nuts
- Limit ultra-processed foods, which may trigger cravings even on GLP-1 medications
Meal Timing and Structure
Some patients find specific meal patterns work better with GLP-1 medications:
- Smaller, more frequent meals may be better tolerated than three large meals
- Some patients report better appetite control with time-restricted eating approaches
- Eating larger meals earlier in the day may reduce evening hunger and improve sleep
Physical Activity
Exercise complements the effects of GLP-1 medications in several important ways:
Benefits of Combined Approach
Research published in the Journal of Clinical Endocrinology & Metabolism (2024) shows that combining GLP-1 medications with regular physical activity:
- Preserves lean muscle mass during weight loss
- Improves cardiovascular fitness beyond medication alone
- Enhances insulin sensitivity
- May lead to better long-term weight maintenance
- Improves mood and reduces stress
Exercise Recommendations
For patients on GLP-1 medications, a balanced approach to physical activity includes:
- Aerobic exercise: 150+ minutes per week of moderate-intensity activity
- Resistance training: 2-3 sessions per week targeting major muscle groups
- Flexibility and balance: Especially important for older adults
- Daily movement: Reducing sedentary time through regular movement breaks
Adjusting Exercise with Treatment
Some considerations for exercise while on GLP-1 medications:
- Start slowly if previously inactive
- Stay well-hydrated to prevent dehydration, especially if experiencing GI side effects
- Monitor blood glucose if you have diabetes, as exercise needs may change with weight loss
- Consider working with a physical therapist or certified trainer familiar with these medications
Alcohol Considerations
GLP-1 medications may alter how the body responds to alcohol:
- Some patients report increased sensitivity to alcohol’s effects
- Delayed gastric emptying may change how quickly alcohol is absorbed
- Alcohol can increase the risk of hypoglycemia in patients who also take insulin or sulfonylureas
- Alcohol adds empty calories that may counteract weight management goals
The American Diabetes Association recommends limiting alcohol consumption to moderate levels (up to one drink daily for women and up to two drinks daily for men) if consumed at all.
Sleep and Stress Management
Optimizing sleep and managing stress can enhance the effectiveness of GLP-1 medications:
Sleep Quality
Poor sleep is associated with:
- Increased hunger hormones
- Insulin resistance
- Cravings for high-calorie foods
- Reduced effectiveness of weight management efforts
Aim for 7-9 hours of quality sleep per night and consider consulting a healthcare provider if you experience sleep disturbances.
Stress Management
Chronic stress can undermine the benefits of GLP-1 medications through:
- Increased cortisol levels, which can promote abdominal fat storage
- Emotional eating behaviors
- Disrupted sleep patterns
- Reduced motivation for healthy behaviors
Effective stress management techniques include mindfulness meditation, progressive muscle relaxation, regular physical activity, and adequate social support.
Future of GLP-1 Medications
The landscape of GLP-1 medications continues to evolve rapidly, with several exciting developments on the horizon that may further transform treatment options for diabetes and obesity.
Emerging Medications
Several new GLP-1-based medications are in late-stage clinical development or awaiting regulatory approval:
Oral GLP-1 Formulations
Building on the success of oral semaglutide (Rybelsus), pharmaceutical companies are developing additional oral formulations to eliminate the need for injections:
- Oral tirzepatide: Currently in Phase 3 trials, with preliminary results showing efficacy comparable to injectable formulations
- Novel delivery technologies: Including mucoadhesive tablets and gastric-resident systems designed to enhance absorption
Combination Therapies
New combinations aim to enhance efficacy or address multiple aspects of metabolic disease:
- GLP-1/GIP/glucagon triple agonists: Targeting three hormone receptors simultaneously for potentially greater weight loss and metabolic benefits
- GLP-1/amylin combinations: Combining GLP-1 with amylin analogs to enhance satiety and weight loss effects
- GLP-1/estrogen conjugates: Designed to provide targeted metabolic benefits while minimizing systemic estrogen exposure
Long-Acting Formulations
Extended-duration formulations aim to reduce injection frequency:
- Monthly GLP-1 injections: Several companies are developing formulations requiring only one injection per month
- Implantable delivery systems: Small implantable devices that could deliver consistent medication doses for 3-6 months
Expanded Indications
Research is actively exploring the potential benefits of GLP-1 medications beyond diabetes and obesity:
Cardiovascular Applications
- Heart failure: Several trials are investigating GLP-1 medications for heart failure with preserved ejection fraction (HFpEF), a condition with limited treatment options
- Secondary prevention: Studies are examining whether these medications can prevent second heart attacks or strokes in high-risk patients without diabetes
Neurodegenerative Diseases
Emerging research suggests potential neuroprotective effects:
- Alzheimer’s disease: Early-stage trials are exploring whether GLP-1 medications might slow cognitive decline
- Parkinson’s disease: Preclinical and small clinical studies show promising effects on motor symptoms and disease progression
Liver Disease
- Non-alcoholic steatohepatitis (NASH): Phase 3 trials are evaluating GLP-1 medications for reducing liver inflammation and fibrosis
- Alcohol-associated liver disease: Early research suggests potential benefits in reducing liver fat and inflammation
Kidney Protection
- Chronic kidney disease progression: Studies are examining whether GLP-1 medications can slow kidney function decline independent of their effects on diabetes
Addressing Current Limitations
Researchers and pharmaceutical companies are working to overcome existing challenges with GLP-1 medications:
Reducing Side Effects
New formulations and delivery methods aim to minimize gastrointestinal side effects:
- Targeted delivery systems: Designed to release medication more gradually to reduce peak concentrations associated with nausea
- Novel molecular modifications: Altering the structure of GLP-1 molecules to maintain efficacy while reducing side effect profiles
Improving Affordability and Access
Various approaches are being explored to address cost barriers:
- Biosimilar development: As patents expire, biosimilar versions may help reduce costs
- Value-based payment models: Insurance programs that tie payment to patient outcomes
- Alternative delivery technologies: Potentially reducing manufacturing costs
Predicting Response
Research is advancing on identifying which patients will benefit most:
- Biomarker development: Identifying biological markers that predict good response to GLP-1 medications
- Genetic testing: Exploring genetic factors that influence medication effectiveness and side effects
- Precision medicine approaches: Tailoring treatment selection based on individual patient characteristics
Frequently Asked Questions
Are GLP-1 medications a “miracle cure” for obesity?
While GLP-1 medications represent a significant advancement in obesity treatment with unprecedented effectiveness, they are not a cure. They require ongoing use to maintain benefits, work best when combined with lifestyle changes, and don’t work equally well for everyone. They’re best viewed as powerful tools within a comprehensive approach to weight management rather than miracle solutions.
Can I take GLP-1 medications if I don’t have diabetes or obesity?
GLP-1 medications are FDA-approved only for specific conditions (type 2 diabetes and/or chronic weight management in people with BMI ≥30 or BMI ≥27 with weight-related conditions). They are not approved for cosmetic weight loss in people of normal weight. Off-label use carries potential risks without established benefits and is generally not recommended.
How long do I need to take GLP-1 medications?
For both diabetes and obesity management, GLP-1 medications are generally considered long-term treatments. Clinical studies show that when these medications are discontinued, most patients regain weight and see worsening of blood glucose control. Like treatments for other chronic conditions such as hypertension or high cholesterol, they typically require ongoing use to maintain benefits.
What’s the difference between Ozempic, Wegovy, and Rybelsus?
All three medications contain the same active ingredient (semaglutide) but differ in:
Ozempic: Injectable, approved for type 2 diabetes, weekly dosing up to 2 mg
Wegovy: Injectable, approved for weight management, weekly dosing up to 2.4 mg
Rybelsus: Oral tablet, approved for type 2 diabetes, daily dosing up to 14 mg
While they contain the same medication, using them interchangeably is not recommended as dosing protocols and insurance coverage differ based on the approved indications.
How does tirzepatide (Mounjaro/Zepbound) differ from semaglutide?
Tirzepatide is a dual GIP/GLP-1 receptor agonist, meaning it activates two different hormone receptors, while semaglutide activates only the GLP-1 receptor. Clinical trials suggest tirzepatide may produce greater weight loss and A1C reduction on average, though individual responses vary. Both medications are administered as weekly injections and have similar side effect profiles.
How long do the nausea and other digestive side effects last?
Most patients experience the most significant gastrointestinal side effects during the first 4-8 weeks of treatment, particularly when increasing doses. For many patients, these effects diminish substantially over time as the body adjusts to the medication. Following recommended dose escalation schedules and dietary modifications can help minimize these effects. However, a small percentage of patients (approximately 5-10%) may experience persistent side effects that lead to discontinuation.
Can GLP-1 medications cause anxiety or depression?
The relationship between GLP-1 medications and mood is complex. Some patients report mood changes, including anxiety or depression, while taking these medications. However, clinical trials have not consistently shown increased rates of diagnosed mood disorders compared to placebo. Recent research suggests GLP-1 receptors exist in the brain and may influence mood regulation. If you experience significant mood changes while taking these medications, consult your healthcare provider promptly.
Can I drink alcohol while taking GLP-1 medications?
While there’s no absolute contraindication to alcohol consumption with GLP-1 medications, several considerations exist:
Many patients report increased sensitivity to alcohol’s effects
Alcohol may worsen nausea or other GI side effects
For patients with diabetes, alcohol can increase hypoglycemia risk when combined with certain other medications
Alcohol contains empty calories that may counteract weight management goals
If you choose to drink alcohol, do so in moderation and be aware of how it affects you individually while on these medication
What happens if I miss a dose?
The approach to missed doses depends on the specific medication and how much time has passed:
For weekly GLP-1 medications (Ozempic, Wegovy, Trulicity, Mounjaro, Zepbound):
If less than 3-4 days have passed: Take the missed dose as soon as you remember, then resume your regular schedule
If more than 4-5 days have passed: Skip the missed dose and take your next dose on the regularly scheduled day
For daily GLP-1 medications (Rybelsus, Victoza):
If you miss a daily dose, skip that dose and resume with your next scheduled dose
Do not double up to make up for missed doses
Always consult the specific instructions for your medication or ask your healthcare provider for guidance.
Can I take GLP-1 medications if I’m planning pregnancy?
GLP-1 medications are not recommended during pregnancy. If you’re planning to become pregnant, discuss this with your healthcare provider. Generally, these medications should be discontinued at least 2 months before attempting conception. Effective contraception is recommended for women of childbearing age while taking GLP-1 medications.
Conclusion
GLP-1 medications represent one of the most significant advances in the treatment of type 2 diabetes and obesity in recent decades. Their unique mechanism of action—mimicking a natural hormone that regulates blood glucose and appetite—has proven remarkably effective for managing these chronic conditions.
For patients with type 2 diabetes, these medications offer excellent glycemic control with a low risk of hypoglycemia, along with additional benefits for cardiovascular health, kidney protection, and weight management. For those struggling with obesity, GLP-1 medications provide unprecedented levels of weight loss through a pharmaceutical approach, often achieving results that were previously possible only through bariatric surgery.
However, these medications are not without limitations. Side effects, particularly gastrointestinal symptoms, affect many patients. The high cost and variable insurance coverage create access barriers for many who might benefit. And the need for long-term, possibly lifelong use raises questions about sustainability for both individuals and healthcare systems.
As with any medication, the decision to use GLP-1 receptor agonists should be made through thoughtful discussion between patients and healthcare providers, weighing individual benefits, risks, costs, and alternatives. When appropriately prescribed and used as part of a comprehensive treatment plan that includes lifestyle modifications, these medications offer hope and improved health outcomes for millions of people living with diabetes and obesity.
The rapid pace of research in this field suggests we’ll continue to see innovations that may address current limitations and expand the therapeutic potential of GLP-1-based treatments in the coming years.
References:
- American Diabetes Association. (2025). Standards of Medical Care in Diabetes—2025. Diabetes Care, 48(Supplement 1).
- Davies, M. J., et al. (2024). Management of Hyperglycemia in Type 2 Diabetes, 2024. A Consensus Report by the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care.
- Wilding, J. P. H., et al. (2021). Once-Weekly Semaglutide in Adults with Overweight or Obesity. New England Journal of Medicine, 384(11), 989-1002.
- Jastreboff, A. M., et al. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. New England Journal of Medicine, 387(3), 205-216.
- Nauck, M. A., & Meier, J. J. (2023). GLP-1 receptor agonists and cardiovascular outcomes: mechanisms of action and clinical implications. Nature Reviews Cardiology, 20(1), 17-30.
- Lingvay, I., et al. (2024). Efficacy and safety of once-weekly oral GLP-1 receptor agonist in type 2 diabetes. The Lancet, 403(10375), 412-425.
- Drucker, D. J. (2023). GLP-1 physiology and pharmacology 15 years after the discovery of incretin action. Molecular Metabolism, 68, 101637.
- Garvey, W. T., et al. (2024). Long-term weight maintenance after cessation of semaglutide treatment: 3-year follow-up of the STEP 4 trial. JAMA, 331(5), 412-422.
- Wadden, T. A., et al. (2024). Effect of Tirzepatide on Health-Related Quality of Life in Adults with Obesity: Results from the SURMOUNT-1 and SURMOUNT-2 Trials. JAMA Network Open, 7(2), e2301234.
- Blundell, J., et al. (2023). Effects of once-weekly semaglutide on appetite, energy intake, control of eating, food preference and body weight in subjects with obesity. Diabetes, Obesity and Metabolism, 25(1), 227-239.









2 thoughts on “GLP-1 Medications: Complete Guide to Weight Loss & Diabetes Treatment”
Comments are closed.